- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
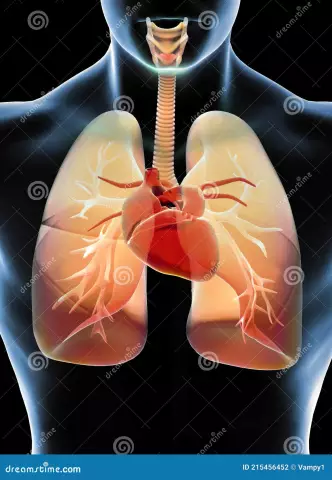
Chronic heart failure, the symptoms of which will be described below, is a pathology, the manifestations of which are associated with impaired blood supply. The condition is noted at rest and during exercise and is accompanied by fluid retention in the body. Treatment of cardiovascular diseases in the majority is carried out medically and comprehensively. Timely access to a doctor contributes to a more rapid restoration of blood supply and the elimination of pathology. Next, let's take a closer look at what CHF is. The classification of the disease, signs and therapeutic measures will also be described in the article.

General information
CHF, the classification of which is quite extensive, is based on a decrease in the ability of the organ that pumps blood to empty or fill. This condition is primarily due to muscle damage. Equally important is the imbalance of systems that affect cardiovascular activity.
Clinical picture
How it manifests itselfchronic heart failure? Symptoms of pathology are as follows:
- Shortness of breath - shallow and rapid breathing.
- Increased fatigue - reduced tolerance for normal physical activity.
- Peripheral edema. As a rule, they appear on the legs and feet, over time they rise higher, spreading to the thighs, the anterior wall of the peritoneum, the lower back, and so on.
- Rapid heartbeat
- Cough. At the initial stages, it is dry, then scanty sputum begins to stand out. Subsequently, blood inclusions may be detected in it.
- Orthopnea position. The patient has a need to lie with his head elevated (on pillows, for example). In a flat horizontal position, shortness of breath and coughing begin to increase.

Forms of pathology
Despite therapeutic measures, the patient's condition may worsen. In this case, a more thorough diagnosis of the heart and circulatory system is necessary. Deep research will reveal hidden provoking factors. The following stages of CHF are distinguished:
- First (initial). At this stage of CHF, there are no circulatory disorders. Echocardiography reveals latent dysfunction in the left ventricle.
- Second A (clinically expressed). The condition is characterized by impaired hemodynamics (blood flow) of one of the circles.
- Second B (heavy). This stage is characterized by a violation of hemodynamics in both circles. Damage to the structure of the organ and blood vessels is also noted.channels.
- Second (final). The condition is accompanied by hemodynamic disturbances of a pronounced nature. Severe, often irreversible changes in the structure of target organs are also characteristic of this form of CHF.
Classification of pathology can also be carried out according to functional type. There are four in total.

Functional types
As in the previous division, changes can be both for improvement and deterioration even against the background of ongoing therapeutic measures in case of detected CHF. The classification according to functional types is as follows:
- The first type is characterized by the lack of restriction of physical activity. The patient can endure the physical activity habitual to the body without showing signs of pathology. Slow recovery or shortness of breath may occur with overexertion.
- The second type is characterized by limited activity to a slight extent. Pathology does not manifest itself in any way at rest. The usual, habitual physical activity of the body is tolerated by patients with shortness of breath, increased fatigue or increased rhythm. At this stage, cardiac diagnostics is highly recommended.
- In the third type, there is a more noticeable limitation of activity. Unpleasant sensations in the patient at rest are absent. Less intense than usual physical activity is accompanied by the manifestation of signs of pathology.
- In the fourth type, any activity of the patient is accompanied by the appearance of unpleasant sensations. Signs of pathologyobserved in the patient at rest, intensifying with little physical activity.
Zones of blood stasis
Depending on the predominant localization of the disorder, the patient may have:
- Right heart failure. In this case, stagnation is noted in a small circle - the pulmonary blood channels.
- Left ventricular failure. In this case, stagnation is localized in a large circle - in the blood channels of all organs, except for the lungs.
- Biventricular (biventricular) failure. Blood stasis in this case is observed in two circles at once.

Phases
Treatment of cardiovascular diseases is selected in accordance with the clinical picture. Manifestations of pathologies depend on the localization of disorders and provoking factors. Of no small importance in the selection of therapy is the history of the disease. CHF may be associated with impaired diastole and/or systole. In accordance with this, several phases of pathology are distinguished. In particular, there is:
- Systolic heart failure. It is associated with a disorder of systole - the time of contraction of the ventricles.
- Diastolic insufficiency. This phase is caused by a violation of diastole - the time of relaxation of the ventricles.
- Mixed shape. In this case, there are violations of diastole and systole.
Reasons
When choosing a therapeutic method to eliminate CHF, degrees, phases and forms are of great importance. However, it is also important to identify the causes of developmentpathology. Chronic heart failure may result from:
- Myocardial infarction. In this condition, the death of part of the heart muscle occurs, which is associated with the cessation of blood flow to it.
- CHD in the absence of a heart attack.
- Arterial hypertension - persistent increase in pressure.
- Taking drugs. In particular, pathology can develop as a result of the use of anticancer drugs and medications to restore the rhythm.
- Cardiomyopathy - lesions of the heart muscle in the absence of pathologies of the organ's own arteries and lesions of its valves, as well as arterial hypertension.
- Diabetes mellitus.
- Thyroid lesions.
- Adrenal dysfunction.
- Obesity.
- Cachexia.
- Lack of a number of trace elements and vitamins.
- Amyloidosis.
- Sarcoidosis.
- HIV infections.
- Terminal kidney failure.
- Atrial fibrillation.
- Heart blockade.
- Exudative and dry pericarditis.
- Congenital and acquired heart defects.

Detection of pathology
The diagnosis of "CHF" is made on the basis of an analysis of complaints and anamnesis. In a conversation with a doctor, the patient should be told when the signs of pathology appeared and what the patient associates them with. It also turns out what ailments the person and his relatives had. The specialist needs to know about all medications taken by the patient. On physical examination, skin color and swelling are assessed. When listeningheart is determined whether murmurs are present. The presence of stagnation in the lungs is also detected. As obligatory researches the analysis of urine and blood is appointed. Studies can detect comorbidities that may affect the course of CHF. Treatment in this case will be comprehensive, aimed at eliminating background ailments. A biochemical blood test is also prescribed. The results determine the concentration of cholesterol and its fraction, urea, creatinine, sugar, potassium. Testing for thyroid hormones. The specialist may prescribe an immunological study. During it, the level of antibodies to heart tissue and microorganisms is determined.
Research using equipment
ECG allows you to assess the rhythm of heartbeats, determine rhythm disturbances, the size of the organ, and also identify cicatricial changes in the ventricles. A phonocardiogram is used for noise analysis. With its help, the presence of systolic or diastolic murmur is determined in the projection of the valves. Plain radiography of the sternum is used to assess the structure of the lungs and heart. This study also allows you to determine the size and volume of the departments of the organ that pumps blood, to determine the presence of congestion. Echocardiography is used to study all parts of the heart. During the procedure, the thickness of the walls of departments and valves is determined. Also, with the help of echocardiography, it is possible to determine how pronounced the increase in pressure in the pulmonary vessels is. Analysis of the movement of blood is carried out during the Doppler echocardiography. The doctor may prescribe other studies inaddition to those described.

CHF treatment: recommendations
First of all, the patient is prescribed a special diet. In the diet, the amount of table s alt is limited to three grams and liquids to 1-1.2 liters per day. Products should be easy to digest, be high in calories, contain vitamins and protein in the required amount. The patient should be weighed regularly. Weight gain of more than 2 kg within 1-3 days, as a rule, indicates fluid retention in the body and decompensation of CHF. Treatment may include psychological help. It aims to speed up the recovery of the patient. Psychological assistance can also be provided to relatives of the patient. For patients, it is undesirable to refuse loads completely. The level of activity for each patient is determined individually. Preference should be given to dynamic loads.
Main drug therapy
Drugs for heart failure are divided into groups: basic, additional and auxiliary. The first includes:
- ACE inhibitors. They help slow down the progression of pathology, protect the heart, kidneys, blood vessels, and control blood pressure.
- Angiotensin receptor antagonists. These drugs are recommended for intolerance to ACE inhibitors or together with them in combination.
- Beta-blockers (drugs "Concor", "Anaprilin" and others). These tools provide control over pressure and frequencycontractions, have an antiarrhythmic effect. Beta-blockers are prescribed together with ACE inhibitors.
- Diuretics (preparations "Amiloride", "Furosemide" and others). These products help to eliminate excess fluid and s alt from the body.
- Cardiac glycosides. These drugs are prescribed mainly in small doses for atrial fibrillation.
Additional funds
- Satines are prescribed if IHD is the cause of CHF.
- Indirect anticoagulants. The drugs of this group are prescribed with a high probability of thromboembolism and with atrial fibrillation.

Ancillary medicines
These funds are prescribed in special cases, with severe complications. These include:
- Nitrates. These drugs improve blood flow and dilate blood vessels. Medicines in this group are prescribed for angina pectoris.
- Calcium antagonists. These medicines are indicated for persistent angina pectoris, arterial hypertension (persistent), increased pressure in the pulmonary blood channels, pronounced valve insufficiency.
- Antiarrhythmic drugs.
- Disaggregants. These drugs have the ability to impair clotting by preventing platelets from sticking together. Medicines of this group are indicated in the secondary prevention of a heart attack.
- Inotropic non-glycoside stimulants. These funds are used for a marked decrease in blood pressure and heart strength.
Surgical methods
In the absence of the effectiveness of drug exposure, surgical, mechanical intervention is used. In particular, the patient may be prescribed:
- Coronary artery bypass grafting. The operation is performed with severe atherosclerotic vascular damage.
- Surgical correction of valve defects. Intervention is carried out in case of severe stenosis (narrowing) or valve insufficiency.
-
Organ transplantation. A heart transplant is quite a radical measure. Its implementation is associated with a number of difficulties:
- probable rejection;
- insufficient number of donor organs;
- The use of artificial devices that provide circulatory support. They are injected directly into the patient's body. Through the skin surface, they are connected to batteries located on the patient's belt. However, the use of devices is also accompanied by problems. In particular, infectious complications, thromboembolism and thrombosis are likely. Prevents more extensive use of devices and their high cost.
- Using an elastic mesh frame. They envelop the heart with dilated cardiomyopathy. This measure makes it possible to slow down the increase in the size of the organ, increase the effectiveness of the drug effect, and improve the patient's condition.