- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
Deterioration of vision in hypertension is a secondary phenomenon. It is associated with changes in the blood vessels. The degree of damage to the organs of vision can be different and manifests itself in the form of edema of the nipple of the optic nerve, hemorrhages, detachment, necrosis of the retina and other degenerative processes. The eyes, along with the kidneys, brain and blood vessels, are the target organs most affected by hypertension.
The eyes are a mirror of cardiovascular pathologies
According to various experts, a change in the day of the eye in hypertension is observed in 50-95% of patients. Periodic examinations by an ophthalmologist are one of the mandatory types of diagnostic studies for such patients. Control over the state of target organs is carried out for such purposes as:
- determining the prognosis of arterial hypertension (AH);
- control of the course of the disease and deterioration of vision;
- efficacy and safety assessmenttherapeutic techniques.
In modern international recommendations for the management of patients with arterial hypertension, a system of criteria characterizing the risk and degree of damage to various organs in hypertension is constantly updated and developed. Changes in the fundus of the eye in hypertension are of particular importance in the initial stages of this disease, since deterioration is often asymptomatic.
The blood supply to the optic nerve inside the orbit is through the posterior ciliary arteries. The retinal central vein provides blood circulation in the retina. Violation of blood flow under the influence of adverse factors leads to a deterioration in the metabolism in the retina and optic nerve.
Classification
Change in the fundus in hypertension goes through several stages (Keith-Wagner classification):
- Scattered or segmental, mild narrowing of small blood vessels and arteries. No hypertension (high blood pressure).
- Stronger vasoconstriction, displacement of the retinal veins into its deeper layers, the formation of decussations with arteries due to the pressure of the arterial walls.
- Retinal damage due to severe vascular disorders (its edema, small and large hemorrhages, the appearance of bloodless foci such as "cotton patches"). The general condition of the patient is characterized by impaired cardiac and renal activity, high hypertension.
- Deterioration or complete loss of vision due to severe narrowing of the arteries and arterioles, swelling of the retina and optic discnerve (ON), the appearance of solid exudates around it. Serious condition of the patient.

This classification was first proposed in 1939 and is currently the most common in medical practice. At the same time, it was proved that the condition of the fundus vessels in hypertension is a prognostic parameter of lethal outcome in patients with hypertension. The disadvantages of this classification include difficulties in determining the initial stage of damage to the retina (retinopathy), the lack of a clear relationship between the stages and severity of hypertension. Some signs may develop inconsistently, which is associated with the individual characteristics of the blood supply to the organs of vision.
Occurrence of retinopathy
Changes in the fundus under pressure are due to the following mechanisms:
- Short-term narrowing of small blood vessels at the initial stage as a result of triggering the mechanism of blood flow autoregulation. An increase in blood velocity as a result of an increase in pressure. Change in vascular resistance as a result of the adaptive ability of the body to maintain a stable blood flow.
- Thickening of the inner layer of arteries and veins due to chronic increase in vascular pressure, active neoplasm of smooth muscle fibers and destruction of fibrillar protein. Generalized narrowing of small arteries.
- With the growth of destructive processes, large molecules penetrate from the blood vessels into the retina, deathcells of smooth muscle tissue and the layer lining the arteries. The blood supply to the retina is significantly worsened.
Diagnosis
Examination of the fundus for hypertension is carried out by two main methods:
- Ophthalmoscopy - an examination with an ophthalmoscope, which is included in the standard diagnosis by an ophthalmologist
- Fluorescein angiography. Before the procedure, a special substance, sodium fluorescein, is injected intravenously. A series of photographs is then taken while being irradiated with a light source, as a result of which this compound begins to emit electromagnetic waves. Normally, the dye does not penetrate beyond the vascular wall. If there are defects, they become visible in the picture. The duration of the procedure is about half an hour.
In older people over the age of 65, hypertensive syndrome can be misdiagnosed as retinal hemorrhages and fluid leakage through the blood vessels are often due to other causes. According to some data, the diagnosis of hypertension, based on the results of an ophthalmological examination, is correct only for 70% of patients. At the late stage of the disease, the absence of specific changes in retinal vessels is observed only in 5-10% of patients.
Differential diagnosis during the study of the fundus in hypertension is carried out with pathologies such as:
- diabetes mellitus;
- consequences of radiation exposure;
- obstruction of the lumen of the veins and carotid artery (ocular ischemic syndrome);
- diseases of the connective tissue.
The key sign of hypertensive retinopathy is a change in blood pressure.
Description of the fundus in hypertension
In ophthalmology, there are 2 types of changes in the fundus - with and without retinopathy. In the first case, initial transformations of the vascular network are observed, the arteries still have a rectilinear course, but their walls are already becoming dense and press on the veins, reducing their lumen. With a long-term condition, retinopathy occurs, which is complicated by hemorrhages and exudate secretions from small arteries.
The following pathological processes occur in the fundus of the eye with hypertension:
- angiopathy;
- arteriosclerosis;
- retino- and neuroretinopathy.
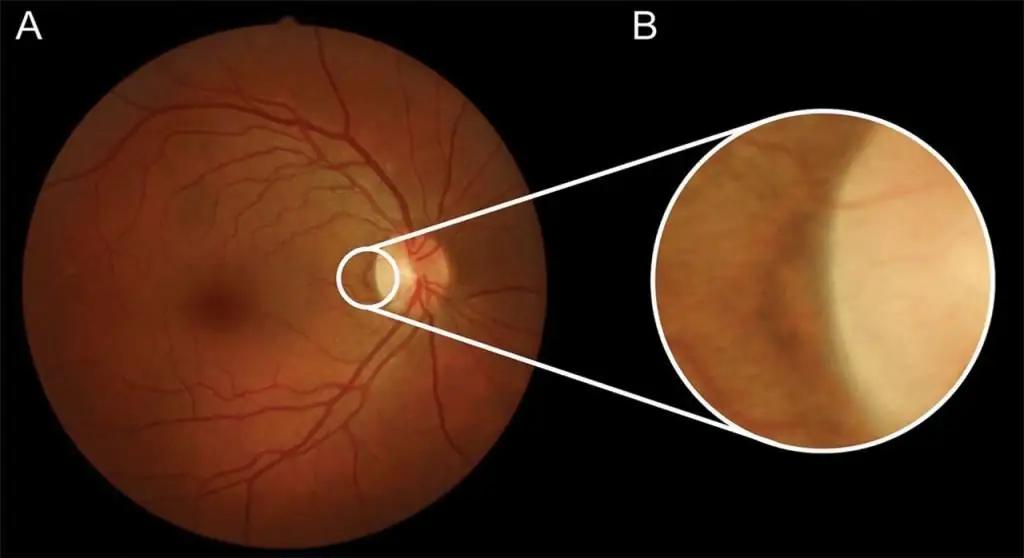
Patients with high blood pressure can develop retinal infarction, which leads to permanent visual impairment. The inner surface of the eye normally looks like this:
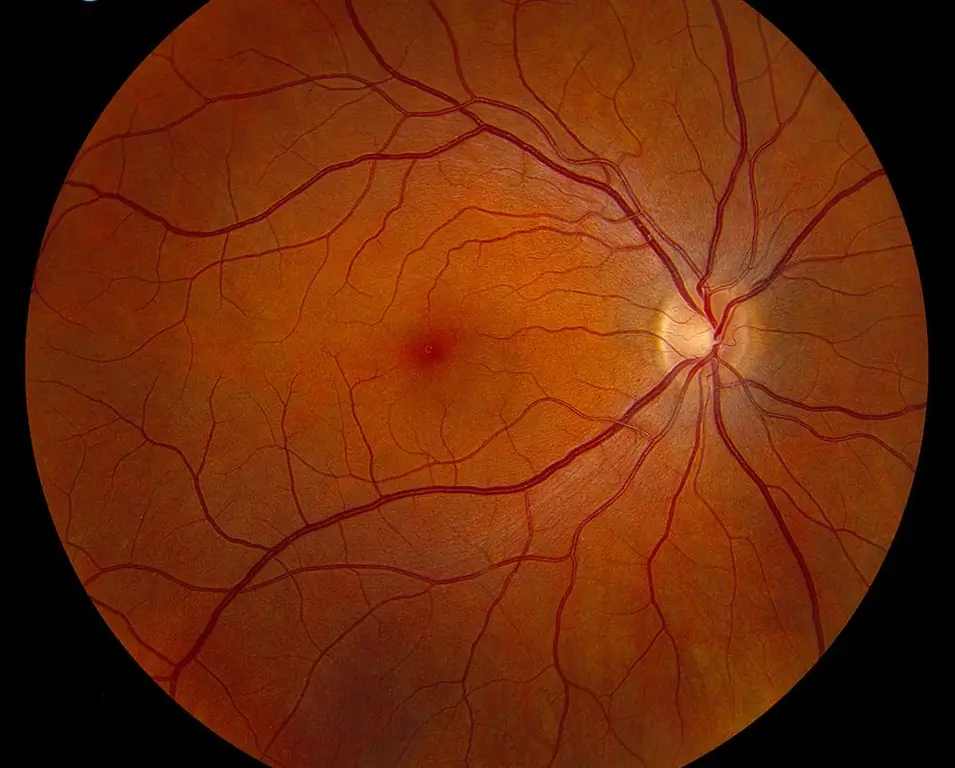
A photo of the fundus in hypertension, depending on the nature of the lesions, is presented below.
Changes in blood vessels
At the bottom of the eye, 2 vascular trees stand out: arterial and venous, which are characterized by several parameters:
- expressiveness;
- branching and its features;
- ratio of diameters (normal arterio-venous ratiois 2:3; with hypertension it decreases);
- tortuosity of branches;
- light reflex.
With hypertension, the arteries often become less "bright", the pattern of blood vessels becomes poorer (the same phenomenon is observed with myopia). This is due to a decrease in the intensity of blood flow. With increasing age, the arterial tree also looks less visible due to the thickening of the vessel wall. The veins, on the other hand, acquire a darker color and are better visualized. In some patients with good vascular elasticity, plethora is observed in both the arterial and venous tree.
Narrowing of the arteries during the study of the fundus in hypertension, observed only in half of the patients. It may have the following features:
- arterial asymmetry in the right and left eye;
- uneven cross-section of one artery in the form of a chain of clamping and dilated sections;
- change only individual branches.
In the initial stages of hypertension, this is due to uneven contraction of blood vessels in different areas, and during the period of sclerotic changes, when functional tissues are replaced by connective tissue, this is due to local thickening of the vessel walls. Prolonged hypertension leads to chronic hypoxia of the retina, disruption of its functions, proteinaceous dystrophy.
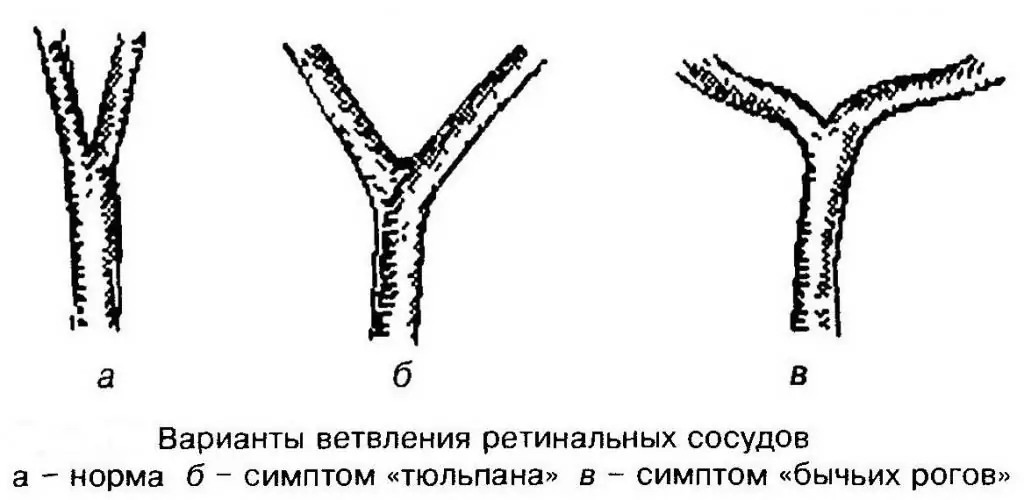
Mutual positioning
One of the common symptoms of angiopathy is a violation of the normal branching and arrangement of blood vessels in the fundus with hypertension. In a he althy person, the arteries are divided into twoequal branches that diverge at an acute angle. In patients with hypertension, this angle is increased (a sign of "bull horns"). This occurs due to increased pulse beats of the blood. An increase in the angle of divergence contributes to a slowdown in blood flow in this area, which leads to the following negative consequences:
- sclerotic changes;
- blockage of blood vessels;
- destruction of the arterial wall due to lateral and longitudinal stretching.
One of the most important and most common diagnostic signs of fundus disorders in hypertension is the decussation of arteries and veins, called the Gunn-Salus sign. However, this phenomenon is also characteristic of arteriosclerosis without hypertension.
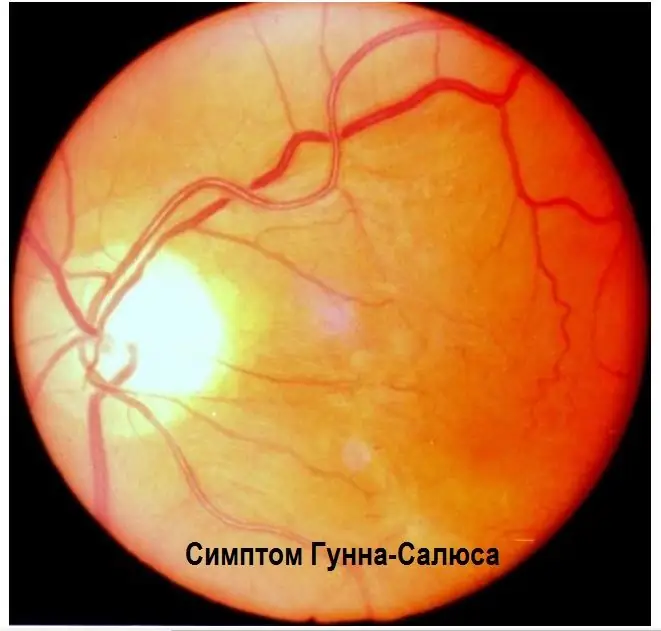
In this case, the venous blood vessels are squeezed. This phenomenon develops in 3 stages:
- narrowing of the diameter of the vein under the artery;
- squeezing the vessel and its displacement deep into the retina;
- full venous compression, no visualization of the blood vessel.
Retinal arteriosclerosis
Characteristic symptoms of retinal lesions in hypertension associated with retinal arteriosclerosis are as follows:
- The appearance of light stripes running along the vessels (in ophthalmology they are called "cases"). This phenomenon is associated with a thickening of the vascular wall and a deterioration in its translucency.
- Wide and less bright reflex on arterial vessels.
- Syndrome of "copper wire" (yellow tint, detected mainly on large branches) and "silver wire" (bright white glow, which most often occurs on small arteries, the diameter of which does not exceed 50 microns).
The appearance of a light reflex along the vessels is explained by sclerotic changes in them, impregnation of their walls with exudate, as well as deposits of fat-like substances. Vessels at the same time become pale and seem empty.
Hemorrhages
Hemorrhages in the fundus of the eye with hypertension appear due to the following reasons:
- leakage of blood cells through a broken vascular barrier;
- rupture of an aneurysm (a place where the wall of an artery stretches and bulges) under the influence of high blood pressure;
- microthrombosis.
Most often they appear near the optic disc in the form of radially directed strokes, "tongues of flame" and stripes. In the central region of the retina, hemorrhages are also located radially to the periphery. Less commonly, hemorrhages form in the nerve fiber layer in the form of spots.

Exudates
Another sign of negative changes in the fundus of the eye in hypertension are exudates of gray-white color, soft, loose consistency, reminiscent of cotton wool. They develop rapidly over several days, but do not merge with each other. At their core, these formations represent an infarction of the layernerve fibers, resulting from the deterioration of blood flow in the blood vessels. There is a violation of the connection between the body of the neuron and its end. Nerve fibers swell and then collapse. These necrotic processes are also characteristic of other pathologies:
- diabetic retinopathy;
- blockage of the lumen of the central retinal vein by a thrombus;
- congestive ONH, or swelling of the eye disc in the absence of inflammation, resulting from a slowdown in the flow of fluid from the eyeball to the brain (this condition can occur when intracranial pressure changes).
The structure of solid exudates in the retina includes fats, high molecular weight proteins, remnants of cells and macrophages. These formations can be of various shapes and sizes. Their appearance is associated with the penetration of blood plasma through the walls of small blood vessels and the degeneration of surrounding tissues. Exudates may spontaneously resolve within a few months if there is a trend of improvement.
Edema formation
The occurrence of retinal edema and optic disc in the fundus of the eye with hypertension indicates a malignant course of hypertension. The accumulation of edematous fluid due to impaired blood supply leads to an increase in protein content. As a result, the retina becomes opaque.
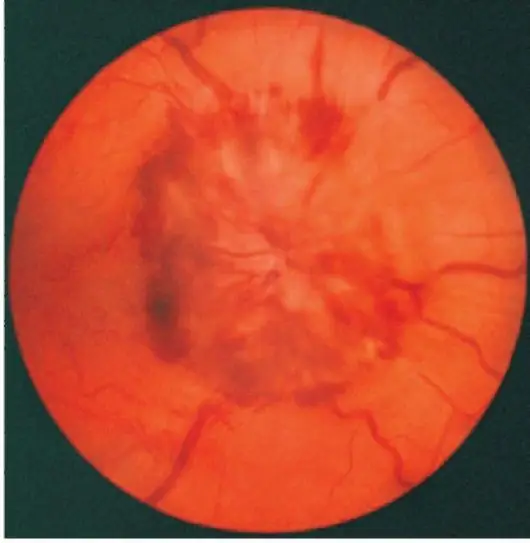
Edema of the optic nerve can be in various forms - from mild to the development of congestive ONH syndrome with hemorrhages, exudates in the central zone of the retina andfoci of local infarction.
The set of signs of angiopathy described above, edema, hemorrhages and exudates are a typical picture of hypertensive neuroretinopathy (non-inflammatory lesions of the retina and optic nerve). In its late stage, irreversible destruction of the vitreous body is observed.
Visual functions
One of the first subjective signs in hypertension is impaired adaptation of vision in the dark. In more rare cases, the patient may notice that visual acuity has deteriorated. This is due to hemorrhages and swelling in the central part of the retina. Instrumental research also shows the following changes that occur in the fundus of the eye with hypertension:
- constriction of visual fields;
- shift of lines corresponding to areas of the retina with the same light sensitivity;
- expansion of the “blind spot”, an area of the retina insensitive to light rays (the exit point of the optic nerve);
- scotomas - areas of the visual field where it is weakened or absent altogether.
The decrease in visual acuity in retinopathy in the first and second stages is usually insignificant. In the last stages, it is more pronounced due to retinal edema and its detachment. The danger of eye diseases as complications of hypertension lies in the fact that when negative processes become noticeable to the patient, then surgical correction of vision is often ineffective.
Prevention
Prevention and main directions of eye treatment in hypertension are associated with the treatment of the underlying disease. Pressure correctioneven in advanced stages, it can improve visual acuity (most often with residual visual loss).
There are 2 types of prevention:
- Primary. It is intended for he althy people who are at risk for the occurrence of hypertension (hereditary predisposition, sedentary lifestyle, frequent physical and emotional overload, drinking and smoking, kidney disease, obesity, postmenopausal women). If at least one of the risk factors is present, even if the pressure does not exceed normal values, it is recommended to start the preventive measures listed below.
- Secondary - maintaining optimal blood pressure levels with medicines prescribed by a doctor and lifestyle changes as recommended by primary prevention. Secondary prevention is carried out in those people who have already been diagnosed with hypertension.
The preventive package of measures includes the following recommendations:
- reduce s alt (no more than 1 teaspoon per day), alcohol (no more than 20g and 30g for women and men respectively);
- control over body weight and, if necessary, its adjustment (the ratio of height in cm to weight in kg should be in the range of 18-25);
- doing moderate endurance exercise (walking, swimming, running, cycling), increasing their intensity to 3-5 sessions per week;
- eating natural food without preservatives, increasing the amount of fruits and vegetables in the dietdiet, reducing fats of animal origin, starchy foods and sweets (since they contribute to obesity);
- increasing stress resistance through psychological training, sports, hobbies, communication with pets;
- giving up bad habits.
Since negative changes in the fundus of the eye during hypertension are asymptomatic in the initial stages, it is necessary to undergo regular examinations with an ophthalmologist (1-2 times a year).






