- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
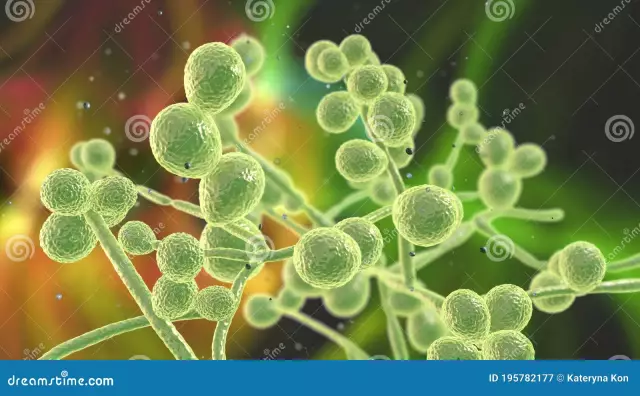
The way the world works is that each of us is surrounded by thousands of microscopic creatures. We do not see them with the naked eye, but we come into contact with them every minute. Some "invisibles" help us, others kill, and still others can bring both harm and benefit. Yeast-like fungi of the genus Candida are just such microbes that do not prevent us from living happily, but in certain situations they begin to behave aggressively, causing candidiasis or thrush. Because these microorganisms are not always harmful, they are called opportunistic pathogens. In total, 186 species of fungi from the genus Candida have been discovered, but only two dozen species are dangerous. They will be discussed in this article.
Candida fungus genus: characteristics
Candida belongs to the genus of yeast. Most of their species are completely harmless, they live in the body of kombucha, in kefir, in other fermented milk products, as well as in the human gastrointestinal tract, being part of the microflora of a he althy intestine. Mushrooms of the genus Candida are aerobes, that is, they lead an active life in the presence of oxygen. They canexist in two forms - yeast and micellar.

In yeast fungi are round or oval blastospores and reproduce by budding. In micellar form, fungal cells elongate, turning into pseudomycelium. Unlike the true one, there are no partitions in it, but there are constrictions. Blastospores are located on them, and chlamydia spores with a double membrane are located on the terminal extensions. In micellar form, mushrooms are able to mate.
Mushrooms of the genus Candida differ from other dimorphic creatures in that they can be in the body of their owner in two of their forms at once, and not change them depending on the temperature of the environment.
An important property of candida is that they can ferment m altose and glucose.
Candidiasis disease, according to recent studies, is caused by approximately 20 species of these fungi, and the most dangerous are C. Albicans (60%) and C. Tropicalis (20%). The remaining 18 species are less widespread and do not have a significant impact on the incidence of candidiasis.
Brief description of pathogenic species
The most widely found fungi of the genus Candida, called C. Albicans. About 8 people out of 10 are their carriers. Basically, these fungi enter the baby's body at birth and live, without causing inconvenience, in the oral cavity, in the esophagus and in the intestines. In women, they are also part of the microflora of the vagina. It is this type of candida that is most often to blame for the occurrence of candidiasis.
The second dangerous species is called C. Tropicalis. These fungi are able to penetrate into the blood andwith its help to populate peripheral organs. Recent studies have revealed the ability of Candida C. Tropicalis to work in tandem with Serratia marcescens and Escherichia coli, and lead to Crohn's disease.
Not very common, but considered the most dangerous yeast fungi of the genus Candida species C. Krusei. They are resistant to the drug Fluconazole, which is used in the treatment of fungal infections, so it is important to correctly differentiate the type of pathogenic fungus that affected the patient.

Candida species C. Glabrata fungi were considered non-pathogenic. They exist only in yeast form and reproduce only by budding. Most often, Candida Glabrata is found on urinary catheters, where it forms thin biofilms. This fungus causes urogenital candidiasis.
Candida C. Parapsilosis often causes sepsis. It can infect wounds, especially if foreign objects get into them.
Fungi species C. Rugosa and C. Lusitaniae and others from the genus Candida are extremely rare. For example, C. Lusitaniae was detected in only 30 patients between 1979 and 1990.
Routes of infection
Conditionally - pathogenic yeast-like fungi of the genus Candida in the process of evolution have developed mechanisms that help them lead a parasitic existence. They are able to withstand freezing and drying for a long time. They can enter the human body with unwashed and insufficiently processed food, with dirty hands and other objects, for example, C. Parapsilosis fungi infect woundswhen foreign objects penetrate into them, including unsterilized medical instruments, and C. Glabrata fungi with urinary or intravenous catheters. Most often, infection with fungi of the species C. Albicans occurs, and from the first minutes of a baby's life. This happens during childbirth if the mother's vagina is colonized by these microbes. There is also an assumption that C. Albicans penetrates the baby's body even at the stage of the embryo, since the fungi have been repeatedly found in the amniotic fluid. If a woman in labor is included in that small percentage of people who are not carriers of mushrooms, her baby during the first years of life can become infected with them through a pacifier, toys, and so on. You should not panic because of this, since candida, once in the body of their host, behave quietly, even help him by controlling the growth of other pathogens.

When Candida infection becomes a disease
A person can be a carrier of these microbes all his life, while remaining completely he althy. Fungi of the genus Candida become pathogenic only when their reproduction is out of control. Reasons:
- pregnancy;
- various infections;
- exacerbation of chronic diseases;
- hypo- or beriberi;
- long-term antibiotic treatment;
- taking corticosteroids;
- hormonal disorders.
The main cause of candidiasis is low immunity. This condition can appear in many situations, including poor nutrition, poor living conditions,frequent stress.
In addition, the sudden growth of fungi of the genus Candida occurs with the following comorbidities:
- AIDS (or HIV infection);
- diabetes mellitus;
- tuberculosis;
- gastrointestinal diseases;
- diseases of the genitourinary system;
- hypothyroidism;
- some blood diseases;
- vaginosis.
Pathogenicity factors
The size of one fungus of the genus Candida is only 2-5 microns, so they can only be seen with a microscope. Those white or yellowish-grayish films that grow on agar or plaque that is visible on the affected areas of the body are whole colonies of fungi, numbering hundreds of thousands of individual microorganisms. Once in the host organism, how do fungi of the genus Candida behave? Microbiological studies have shown that each fungus tends to begin adhesion, that is, to adhere tightly, one might say, to grow into human epithelial cells. This microbes succeed the easier, the lower the immunity of their victim, and the higher her endocrine disorders. The most active fungus in terms of adhesion is C. Albicans. Once on the mucous membranes, it adheres in 100% of cases. The most passive mushroom of the C. Krusei species. It may not be fixed at all, that is, infection does not occur. Help fungi to take root surface proteins, surface proteins and some molecules, such as polysaccharides and glycoproteins, and saliva molecules in the mouth. In general, Candida are glycogenophiles (like glycogen), so they most often colonize tissues where it is abundant, for example, the mucous membranes of the vagina and oral cavity. Atthe occurrence of thrush, fungi of the genus Candida in a smear taken from these organs are detected with a high probability, which makes it possible to accurately diagnose.
At the initial stage of adhesion, fungi are in a yeast form, but quickly rebuild, forming long filaments (hyphae), which more easily penetrate damaged host cells, and are less susceptible to phagocytosis of leukocytes.
Fixed and accustomed, parasites in the course of their life activity secrete various poisons into the host's body:
- candidotoxin (a protein that acts on basophils and mast cells and causes a pseudo-allergic reaction);
- 6 types of low molecular weight toxins (increase vascular permeability, lower blood pressure);
- lipid toxins (cause a local leukocyte reaction and lead to the appearance of granulation tissue).

Candidiasis in children
As noted above, infants become infected with candida either in the womb or at birth during the passage of the birth canal. In the future, the fungus can enter the baby's mouth with a poorly processed nipple, rattles, from the nipples of an infected mother. Symptoms that the baby has contracted thrush are as follows:
- white, curd-like plaque on the tongue, on the inner surface of the gums and cheeks;
- capriciousness;
- refusal of food.
Without treatment, the fungus continues to settle and soon appears on the baby's lips.
Mushrooms of the genus Candida in the intestines are manifested by symptoms of dysbacteriosis, suchlike:
- diarrhea;
- lethargy;
- temperature;
- weight loss.
Diarrhea in infants is dangerous because it leads to rapid dehydration, so a sick child must be hospitalized. Only in a hospital can he be given the necessary treatment (droppers) to prevent fluid loss.
In addition to the digestive tract and oral cavity, thrush in babies can appear on the skin. In this case, not white, but red spots appear, similar to diaper rash. The child becomes very capricious, as any touch of erosion causes him suffering. Most often, skin candidiasis in infants appears in the folds on the legs, on the buttocks and in the groin area. This is preceded by diaper rash, being in a diaper for too long, poor hygiene and inappropriate (synthetic, too tight) clothing.

Treatment of childhood candidiasis
If fungi of the genus Candida have begun a pathogenic process in the child's oral cavity, treatment is usually carried out locally. It consists in the treatment of places where white plaque is observed, with special preparations. Previously, doctors attributed to lubricating the child's mouth with brilliant green. This medicine helps well, but dries the mucous membranes. Now they use "Akriderm", "Fukortsin", solutions of borax in glycerin.
For the purpose of prevention, it is necessary to boil nipples and bottles in the first months of a baby's life, wash rattles. Mom should treat the nipples with antifungal drugs before feeding.
With symptoms of dysbacteriosis, the baby's feces are handed over for bakposev. It is believed that fungi of the genus Candida in the feces of children under 12 months of age may be present in quantities not exceeding 103 CFU / g, and older than 12 months in the amount of 104 CFU / g. If the indicator is exceeded, drugs are prescribed that restore the microflora and strengthen the immune system.
With candidiasis of the skin, the affected areas are lubricated with antifungal ointments - nystatin, levorin. It is very useful to bathe a child with the addition of a decoction of string, calendula, chamomile to the water. All underwear and diapers must be ironed, and diapers should be changed often enough without waiting for them to be completely filled.
If the above treatments do not help, the child is examined further and given antifungal therapy.
Candidiasis in women and men
In adults, Candida fungi can, as in children, infect the mouth, skin, and intestines. Candidiasis in the mouth is manifested by a curdled coating that captures the tongue, gums, palate, inside of the cheeks and is accompanied by painful sensations. Sometimes mucous membranes ulcerate. Candidiasis on the skin is characterized by red spots in the places where the fungus is introduced (under the armpits, under the breasts in women, in the groin, less often under the knees). These spots itch and flake, and ulcerate when scratched.

But most often adults suffer from candidiasis of the genitourinary organs. In women, fungi settle in the vagina and on the vulva, so the disease was called vulvovaginitis. In the initial stages, its symptoms are as follows:
- white (like sour milk) vaginal discharge;
- itching, not passing, but,on the contrary, aggravated after washing and in the morning;
- unpleasant smell of underwear;
- pain during intercourse.
The most telling symptom is Candida in a vaginal swab.
Without treatment, the symptoms get worse. There are pains not only during sexual intercourse, but also with each urination, the vaginal mucosa swells, ulcerates, the discharge becomes thicker.
In men, Candida infection is called balanoposthitis. Symptoms:
- curdled discharge from the penis;
- itching, pain when urinating;
- painful intercourse.
In addition to the genitourinary system, Candida fungi parasitize on the external organs of people. Infection of the nails is called "onychia", and the infection of the nail fold is called "paronychia". The causes of these diseases can be barbs, manicure with infected instruments.
Analysis for fungi of the genus Candida
The presence of candidiasis is determined by the results of such studies:
- smear from the mouth or vagina;
- sowing;
- ELISA;
- PCR.
Additionally, the doctor may order urine and blood tests.
If you plan to take a smear from the vagina and / or urethra, it is not allowed to wash before this, and you can urinate only 2 hours before taking a smear, no later. If a swab is planned to be taken from the mouth, it is forbidden to brush your teeth before this.
For seeding use feces, sputum, urine, scrapings from the affected areas of the skin and mucous membranes. Three days later they receive a response,whether or not the material contains fungi of the genus Candida. The norm is a negative result. If the tests confirm the presence of a fungus, determine its type and sensitivity to medications.
ELISA analysis is called enzyme immunoassay. It helps to identify antibodies to the fungus and track the dynamics of the process. The research material for ELISA is blood from a vein. As a rule, it is carried out in conjunction with bacterial seeding.
The most accurate is the PCR analysis, which means the polymer chain reaction of fungal DNA molecules. It determines the presence of a pathogen even at the very initial stage of the disease. The material for PCR is sputum, secretions, blood.

Treatment
If Candida fungi are found in a patient, treatment is carried out with medication. Inside they write out:
- Fluconazole.
- Nizoral.
- Diflucan.
Ointments are used externally:
- "Clotrimazole".
- "Sertocanazole".
- Miconazole.
- Suppositories with pumafitsin and other drugs that inhibit the growth of the fungus. Anti-inflammatory ointments may also be prescribed.
Treatment of pregnant women is carried out only by external means. Only in some cases is Pumafitsin administered orally.
Urinary tract candidiasis is treated with both sexual partners.
In addition to antifungal drugs, vitamins and other immune-boosting drugs are prescribed.