- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
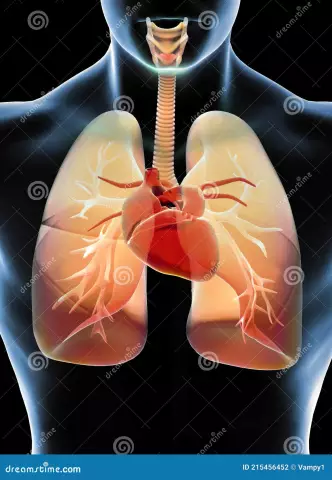
Heart failure is a chronic or acute condition, the cause of which lies in the weakening of myocardial contractility and congestion observed in the systemic or pulmonary circulation.
This is a very dangerous condition. What are the prerequisites for its occurrence and signs of acute heart failure? How is the diagnosis carried out? And, most importantly, how is the treatment carried out?
About the disease
Before studying the signs of acute heart failure, one must have information about this pathology. How is it developing? Due to a decrease in the contractile function of the heart, an imbalance begins to develop between the hemodynamic needs of the body and the capabilities of the heart muscle in their implementation.
This is manifested by an excess of venousinflow to the heart and the occurrence of resistance that the myocardium has to overcome in order to expel blood into the vascular bed.
The cause of acute heart failure is a weakening of the function of any part of the heart (right or left ventricle, or atrium).
This ailment is not independent. It is usually the result of myocardial infarction, aortic valve disease and hypertension. Its formation leads to increased pressure in the capillaries, arterioles and pulmonary veins. Because of this, in turn, the permeability of their walls increases. The result is sweating of the liquid part of the blood. As a result, interstitial leakage is formed, and then alveolar.

Prerequisites and risk factors
What conditions predispose to acute heart failure? Signs of the disease are manifested in various cardiovascular disorders.
Approximately 60-70% of patients with this disease had coronary heart disease and myocardial infarction. Much less often (14%), people with defects are at risk. Approximately 11% of cases occur in patients with dilated cardiomyopathy.
Also a risk factor is advanced age. Among the elderly, in addition to IHD, this disease also causes hypertension (this is about 4% of cases). Many more elderly patients who are faced with signs of acute heart failure suffer from type 2 diabetes mellitus.type, as it turns out in the course of clarifying the anamnesis.
Also, risk factors and possible prerequisites for the development of pathology include:
- Pulmonary embolism.
- Arrhythmia.
- Physical and psycho-emotional overload.
- Hypertensive crisis.
- Pneumonia.
- IHD progression.
- ARVI.
- Kidney failure.
- Anemia.
- Long-term use of cardiotoxic and fluid retention medications.
- Alcoholism.
- Intensive mass gain.
- Increased total circulating blood volume.
- Infectious endocarditis.
- Rheumatism.
- Myocarditis.
All of the above undoubtedly leads to a decrease in the compensatory mechanisms of the heart.

Symptoms
What are the first signs of acute heart failure? There are two most pronounced symptoms: alveolar pulmonary edema and cardiac asthma.
The attack of the second illness is provoked, as a rule, by neuropsychic or physical stress. Occurs at night, because of which a person wakes up in fear. He does not have enough air, his heartbeat goes off scale, his throat begins to be tormented by a cough with sputum that is difficult to expel. This state is supplemented by cold sweat and severe weakness.
In such a situation, you need to take a sitting position and lower your legs. When examining a patient in this condition, pale, grayish skin, severe shortness of breath, cold sweat and cyanosis are found.(acrocyanosis).
Pulse very weak but often full. The borders of the heart are expanded to the left, the tone is very deaf. The rhythm can be described as "gallop". Arterial pressure decreases. If you listen to the lungs, you can identify single dry rales.
Due to the increase in stagnation of the small circle, pulmonary edema develops. A sharp choking accompanies a strong cough, and a copious amount of pink, frothy sputum is also secreted.
Even at a distance, you can hear the bubbling breath and wet rales. In addition, a person's neck veins swell, the skin is covered with cold sweat. The pulse becomes threadlike, frequent and arrhythmic. A variety of moist rales appear. This is not just a clinical sign of acute heart failure, but an emergency that requires intensive care. If a person is not helped, he may die.
Signs in men and women
It should be noted that pathology often manifests itself specifically depending on gender. Of course, most of the signs of acute heart failure in men and women are similar, but there are some differences. And they should be given special attention.
Women develop heart problems later than men. They make themselves felt with the onset of menopause (usually after 50 years). With age, the risk of developing insufficiency increases, and by the age of 65, women are just as susceptible to it as men.
It is impossible not to mention that representatives of the strong half of humanity are more likely to experience heart attacks. And therefore for themtimely diagnosis and competent treatment are incredibly important.
Not all women experience pain as a symptom of heart failure. Many possible symptoms are often almost imperceptible. Manifestations occur immediately before the attack. These are arrhythmia, chest burning, dizziness, cough, nausea with vomiting, digestive problems, as well as weakness and sudden fatigue.

Diagnosis
Since the signs of acute heart failure in women and men are a secondary syndrome that develops against the background of some other disease, the purpose of the diagnosis is appropriate - it is important to identify it as early as possible and prevent its development. Most importantly, deficiency can be prevented, so regular check-ups make sense.
When collecting an anamnesis, attention is necessarily drawn to dyspnea and fatigue. These are early signs of acute heart failure. Diagnosis also involves taking an anamnesis - it is necessary to find out if the patient has hypertension, coronary artery disease, cardiomyopathy, whether he had a rheumatic attack and myocardial infarction.
In addition, the doctor detects ascites, rapid low-amplitude pulse, listens to the third heart sound, determines the displacement of its boundaries.
If there is a suspicion of deficiency, then experts conduct the following studies:
- Analysis for gas and electrolyte composition of blood.
- Detection of acid-base balance.
- Study of indicators of protein-carbohydrate metabolism.
- Determination of the level of creatinine and urea.
- Detection of cardiospecific enzymes.
Of course, an ECG is also prescribed. This procedure helps to determine myocardial ischemia, hypertrophy, arrhythmia. They can conduct bicycle ergometry and a treadmill test (stress activities). They imply a gradually increasing level of load, which is necessary to identify the reserve capacity of the heart function.
Also, patients are shown ultrasound echocardiography. Thanks to it, it is possible to identify the cause, which provoked the appearance of signs of acute heart failure in women and men. The same method allows you to evaluate the pumping function of the myocardium.
Mandatory MRI. This method helps to successfully diagnose acquired or congenital heart defects, coronary artery disease, arterial hypertension and other ailments.
Many more patients are shown x-rays of the chest and lungs. So you can determine cardiomegaly and stagnant processes in the small circle.
Also in the process of diagnosis, it is important to assess the contractility of the ventricles, to identify how spacious they are. For this purpose, radioisotope ventriculography is done.
If there are serious signs of acute heart failure in men or women, then an ultrasound scan of the liver, abdominal cavity, pancreas and spleen is mandatory. This is necessary in order to determine if there are lesions in the internal organs.

Principlestherapy
This pathology is a life-threatening condition, and therefore it is very important to promptly provide qualified medical care when the first signs of acute heart failure appear. The reasons for its occurrence may be different, but the therapy is based on general principles.
What are the actions of resuscitators aimed at? This is:
- Restoration of blood flow through damaged vessels.
- Regulation of heart rate.
- Elimination of pulmonary embolism.
- Restoration of the integrity of the heart muscle (for this, emergency surgery is performed).
- Asthmatic relief.
- Oxygen therapy.
- Pain relief.
- Intensification of contractile activity of the myocardium.
- Decreased blood volume.
- Normalization of vascular circulation.
When you notice signs of acute heart failure, the causes and symptoms of which have been described above, you should immediately call an ambulance. Delay increases the risk of death. If the pathology develops at lightning speed, then the doctors will have a maximum of 30 minutes to carry out resuscitation.
How to provide first aid?
When a person has obvious signs of acute heart failure, first aid should be provided. The algorithm of actions is:
- The patient should be put in a comfortable position, legs down.
- Remove him of clothing that makes it difficult to breathe.
- Provide fresh air.
- Call an ambulancehelp.
- Talk to a person, distract him so that he is conscious. Be sure to calm him down.
- Dip your feet and hands in warm water (slowly), then measure the pressure. If the indicators exceed 90 mm Hg. Art., you need to give him a tablet of nitroglycerin.
- After 15 minutes after the onset of the attack, apply a tourniquet to one thigh. Change the position once every 30-40 minutes (if the doctors are traveling for a long time).
It is important to know that there is always a risk of stopping breathing. In case this happens, proceed as follows:
- Place the person on a flat surface, on their back. Put some kind of roller under your head.
- Put your hands down with your palms, rest them on your sternum (lower third), and begin to jerk 60-65 times per minute.
- Simultaneously perform artificial respiration. If resuscitation is carried out by one person, then his algorithm should be as follows: every 13-15 shocks, take 2-3 breaths. With an assistant, 5 pushes account for 1 breath.
- After half a minute, you need to evaluate how effective the resuscitation was. If everything is done correctly, the pupils will again begin to react to light, and the normal skin color will also be restored.
- Even if all else fails, resuscitation must continue. It will be possible to stop only when the doctors arrive.

Used medicines
When confirming the diagnosis based on signs of acute cardiacinsufficiency, the treatment of pathology is carried out with drugs that are prescribed to a person in this condition. Of course, the approach here is purely individual. But usually they prescribe such means:
- Pressor amines. These are Dobutamine, Dopamine and Norepinephrine. These drugs help to regulate the functionality of the myocardium.
- Phosphodiesterase inhibitors. The best option is Amrinon and Milrinon. They improve the tone of the pulmonary vessels, eliminate signs of pulmonary insufficiency and shortness of breath.
- "Levosimendan". At the moment, this is the only medicine with which you can regulate the work of microfibrils. It is usually prescribed at an early stage of deficiency.
- "Digoxin". It is used to reduce the frequency of ventricular contractions during arrhythmias. But this drug has a lot of side effects, and therefore is rarely used in practice.
- "Nitroglycerin". Taking this remedy relaxes the smooth walls of blood vessels, as a result of which the body's response to increased pressure decreases. It is taken when an attack approaches.
- "Sodium nitroprusside". It is used similarly to "Nitroglycerin". But the drug is serious, it should not be taken more than 4 times a week.
- "Furosemide". It has a vasodilating effect, and also accelerates the outflow of urine. As a result, swelling in the upper and lower extremities is eliminated.
- "Morphine". It is a narcotic analgesic and is used only in extreme cases to increase the vagal effect and short-term optimize the work of the heart. There are many side effectsthe drug is also addictive.
Other drugs may also be prescribed. Be that as it may, all of the above is used only for symptomatic treatment. Heart failure itself cannot be eliminated with these drugs. But it will be easier for the patient to endure this condition.

Cure other manifestations
Studying the essence of the pathology and signs of acute heart failure, you need to know how other manifestations of this disease are eliminated.
With pulmonary edema, for example, it is very important to normalize the pressure in the vessels. This will speed up the permeability of the blood and increase its saturation with oxygen. For these purposes, phosphodiesterase inhibitors are prescribed. Supervised cardio workouts are also recommended.
The main task of doctors is to quickly normalize blood pressure and prevent the development of hypoxia. For these purposes, diuretics are used. In especially severe cases, the notorious morphine is used.
If hypertension and cardiac shock occur, it is important to normalize blood pressure and regulate the pumping function of the heart muscle. Inhibitors of potassium and nitric oxide synthesis will help here. In addition, diuretics or the same nitroglycerin are indicated.
In the event that the conduction of the heart muscle is disturbed, or the sinusoidal impulse disappears, the myocardial reaction is stimulated. Then they resort to pressor amines, and in order to normalize weight, they prescribe a specialized diet. She ismeans avoiding s alty, fatty, fried, and everything that contains cholesterol.
Tachycardia is usually quickly eliminated with Digoxin. However, it is taken with extreme caution.
Also, doctors regulate the concentration of nitrate oxide, calcium and magnesium in the blood. For this purpose, classic antiarrhythmics are prescribed, as well as a consultation with a nutritionist.

Prevention
As you know about the signs, symptoms and treatment of acute heart failure, you need to know about preventive measures. To date, there is no specific prevention of this pathology. All activities that are recommended by cardiologists fit into the generally accepted concept of a he althy lifestyle. What will help improve the condition and minimize the frequency of seizures?
- Regular examinations by a cardiologist, therapist, as well as other highly specialized doctors (it all depends on the presence of certain diseases in a person).
- Quitting smoking and minimizing alcohol consumption. Although it is desirable to impose a "taboo" on alcohol. If there are chronic diseases of any systems or organs, then the ban is mandatory.
- Control your body weight. Do not allow weight gain. Any extra kilogram puts an additional strain on the heart. Therefore, in the event that a person’s weight deviates from the norm, you need to reconsider your diet. A nutritionist will tell you how to do this.
- Moderate exercise. That,how intense they will be depends on the he alth of the person.
- Exclusion of any psycho-emotional overload. This must be taken into account both by the patient himself and by those people who are part of his close circle. You can not bring it to overstrain and provoke stressful situations.
- Compliance with the regime of work and rest. Physical overvoltage is also unacceptable.
- Proper nutrition. Usually, in case of insufficiency, diet No. 10 is prescribed with a low energy value (2300-2500 kcal) and with a high content of proteins and carbohydrates.
- Daily blood pressure monitoring.
In conclusion of the discussion of the signs, symptoms and diagnosis of acute heart failure, it should be noted that the 5-year survival rate for people suffering from this pathology is 50%. But the prognosis is variable, they are affected by the severity of the disease, the accompanying background, lifestyle and the effectiveness of therapy. If the treatment was started in the early stages, then it is possible to fully compensate for the patient's condition, preventing the development of pathological conditions.