- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-06-01 06:18.
Cardiosclerosis is a pathology of the heart muscle, which manifests itself in the growth of connective scar tissue that occurs in the myocardium. The disease is serious, as it leads to deformation of the valves and replacement of muscle fibers. And this is fraught with dire consequences.
Why does this pathology occur? What symptoms indicate its presence? How to deal with it? Well, that's what we'll talk about now.
Classification
First of all, it should be noted that the pathology in question is not an independent nosological unit, but one of the varieties of coronary heart disease (CHD).
Cardiosclerosis, however, is usually considered according to the international classification of diseases. In the Russian Federation, it was introduced into medical practice in 1999. This is a directory divided into headings, where diseases are listed, and all of them are assigned an alphabetic and numeric designation.
The gradation of the diagnosis of cardiosclerosis in the ICD looks like this:
- Diseases of the circulatory system - I00-I90.
- Postmyocardial cardiosclerosis - I20.0-I20.9.
- CHD - I10-I25.
- Atherosclerotic heart disease - I25.1.
- Postinfarction cardiosclerosis - I2020-I2525.
- Chronic CAD - I25.
Well, having briefly read the ICD-10 codes for cardiosclerosis, we can move on to a more important topic. Namely, to consider its types, causes, symptoms and treatment.

Types and forms of the disease
It is impossible not to touch upon this topic. The codes for cardiosclerosis in the ICD-10 were discussed above, but it should be noted that this classification does not contain information about the forms of the disease. And there are only two of them:
- Focal cardiosclerosis. In this case, separate scar areas of different size are formed in the myocardium. As a rule, the pathology of this form occurs as a result of myocardial infarction or myocarditis.
- Diffuse cardiosclerosis. This form is characterized by uniform damage to the myocardium and foci of connective tissue. They are distributed over the area of the entire heart muscle. As a rule, cardiosclerosis of this form occurs with IHD.
It is also customary to distinguish etiological types of the disease. But they are the outcome of the primary disease, which entails the replacement of functional myocardial fibers with scars. In ICD-10, cardiosclerosis of some etiological varieties is highlighted separately. In general, there are three of them:
- Atherosclerotic form. Occurs as a result of the transferatherosclerosis.
- Post-infarction. Formed due to myocardial infarction.
- Myocardial. Is the result of myocarditis and rheumatism.
It is important to note that in rare cases other forms are observed. They may be associated with trauma, dystrophy and other lesions of the heart muscle.

Atherocardiosclerosis
Occurs due to damage to the coronary arteries. The presence of this pathology is indicated by the symptoms of a progressive coronary disease:
- Chest pain due to stress or exercise.
- Shortness of breath.
- Discomfort felt in the lower jaw, arm and back.
- Increased heartbeat. Interruptions are often felt.
- Faints.
- Dizziness, nausea and weakness.
- Blurred consciousness.
- Excessive sweating.
- Edema of the lower extremities.
- Psycho-emotional lability.
As the disease progresses, pulmonary edema or attacks of cardiac asthma, ascites and pleurisy, atrial fibrillation, extrasystole, atrioventricular blockade, atherosclerosis of the aorta and arteries may occur.
To establish a diagnosis, a cardiologist examines the patient's history. It is important to consider whether he had atherosclerosis, coronary artery disease, arrhythmia, previous heart attacks, etc. He will also need to undergo the following diagnostic tests:
- Biochemical blood test. Helps detect elevated levels of beta-lipoproteins and the presence of hypercholesterolemia.
- EKG. Required fordetection of coronary insufficiency, arrhythmia, postinfarction scarring, moderate hypertrophy and intracardiac conduction.
- Echocardiography. Allows you to determine violations of myocardial contractility.
- Veloergometry. With its help, it is possible to clarify how strong the dysfunction of the myocardium is, as well as the state of the functional reserves of the heart.
The patient can also be referred for pharmacological tests, polycardiography, cardiac MRI, ventriculography, 24-hour ECG monitoring, coronary angiography and rhythmocardiography. And to clarify whether there is an effusion, a chest x-ray, ultrasound of the abdominal and pleural cavities is performed.

Postinfarction cardiosclerosis
Continuing to talk about the symptoms of this disease, it is worth paying attention to this form of it. From a medical point of view, this pathology is one of the varieties of IHD. Postinfarction cardiosclerosis is manifested by symptoms of heart failure:
- Increase in pressure in the pulmonary veins, capillaries and arterioles, accompanied by an increase in their permeability.
- Lower exercise tolerance.
- Fatigue.
- Harsh breathing with dry wheezing.
- Alveolar pulmonary edema.
- Cardiac asthma triggered by mental or physical stress.
- Severe shortness of breath, acrocyanosis, cold sweat.
- Pale skin. The integument may have a grayish tinge.
- Increased intracranial pressure.
- Weakeningand increased peripheral pulse.
- Lower blood pressure.
To establish the diagnosis of Cardiosclerosis of post-infarction etiology, the doctor, in addition to taking an anamnesis and studying symptoms, directs the patient to the studies listed above. But, in addition to them, one of the following can also be assigned:
- PET heart. Helps to assess myocardial nutrition, the presence of areas of deficiency, as well as determine the degree of cell viability.
- Physical examination. Allows you to detect a shift down or to the left of the apex beat and weakening at the top of the first tone. In rare cases, a systolic murmur is found on the mitral valve.
- Stress tests (treadmill test and bicycle ergometry) and Holter monitoring. These studies help identify transient ischemia.
Echocardiography is especially informative in this case. It helps to detect left ventricular hypertrophy, dilatation, chronic aneurysm of the heart and contractility disorders.
Myocardial cardiosclerosis
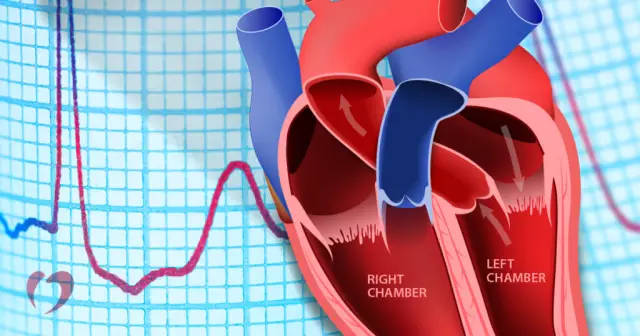
And it is worth talking about this disease separately. Myocarditis cardiosclerosis is a pathology leading to heart failure. In this case, myocardial tissue dies and is replaced by fibrous tissue. Over time, the heart adapts to it, and this leads to an increase in its size. As a result - a violation of blood circulation and insufficiency.
Typically, patients complain of the following symptoms:
- Dizziness.
- Shortness of breath.
- High heart rate.
- Too fastfatigue.
- Heart pains of a squeezing or stabbing character.
- Increase or decrease in heart rate.
- Irregular heart rhythm. They manifest in extrasystole, atrial fibrillation and heart block.
- Aneurysm. This is the name of the expansion and subsequent protrusion of tissue from the wall of the heart. If an aneurysm ruptures, then death cannot be avoided.
To establish the correct diagnosis, the doctor conducts an auscultatory examination, after which he directs him to an ECG and MRI to obtain an image of the heart in several planes. This will allow you to study its condition, as well as examine the valves, walls and chambers.

Other causes of illness
What are the prerequisites for pathologies related to the above forms is clear. But you need to know that there are other causes of cardiosclerosis. Rarer prerequisites for the occurrence of this disease include:
- Radiation exposure. It can penetrate into the thickness of tissues and affect various systems and organs. If the heart muscle is irradiated, the restructuring of the cells occurs at the molecular level.
- Sarcoidosis. This disease is systemic, so it can affect various tissues of the body. If sarcoidosis takes on a cardiac form, then inflammatory granulomas form in the myocardium.
- Hemochromatosis. It is characterized by the active deposition of iron in the heart tissue. Over time, this gives a toxic effect. The result is inflammation, whichbecomes proliferating connective tissue.
- Scleroderma. Connective tissue begins to grow from the capillaries. And the myocardium is rich in them. The heart begins to enlarge as the walls thicken, but there is no evidence of cardiomyocyte destruction or inflammation.
And of course, medicine knows cases when a patient had idiopathic cardiosclerosis. This is a pathology that has formed for no apparent reason. Scientists suggest that the prerequisites are mechanisms that have not been discovered so far.
Perhaps, there are hereditary factors that provoke the growth of connective tissue at a certain life stage. But this probability has so far only been discussed by experts.
Treatment with vasodilators
Much has been said above about the codes of cardiosclerosis according to the ICD, the symptoms of this pathology and diagnostic methods. Now we can talk about exactly how it is treated.
One point needs to be mentioned right away. Cardiosclerosis is a very serious disease. Self-treatment in this case is unacceptable! It is only the doctor who determines which medications will be taken to relieve symptoms, taking into account the results of the diagnosis and the individual case of the patient.
As a rule, vasodilators are often prescribed. These drugs significantly improve local blood circulation. Usually appoint such means:
- Cavinton. Improves brain metabolism and blood circulation. Increases the consumption of oxygen and glucose by the brain tissue. Significantly increases the resistance of hypoxia to neurons and reduces aggregationplatelets, thins the blood. Increases cerebral blood flow. Increases blood supply in those ischemic areas where there is low perfusion.
- "Cinatropil". A combined drug that has a vasodilating, antihypoxic and nootropic effect. Improves metabolism in the central nervous system, cerebral circulation and elasticity of erythrocyte membranes, reduces the excitability of the vestibular apparatus.
They should be taken with cardiosclerosis in periodic courses, 1 tablet 2-3 times a day. The first period of therapy usually lasts 2-3 months.

Heart drugs
These funds exist innumerable, and they are all divided into groups. Some drugs regulate blood circulation and control vascular tone, others reduce pain, some act directly on the muscle, providing anti-sclerotic and hypolipidemic effects, etc.
Cardiosclerosis of the heart is a complex disease, so drugs of different groups are prescribed, and here are the most popular ones:
- Korglikon. A glycoside that has a positive inotropic effect. It has a plant origin, the basis of the drug is an extract of May lily of the valley leaves. Increases the sensitivity of cardiopulmonary baroreceptors, increases the activity of the vagus nerve.
- "Asparkam". Replenishes the deficiency of magnesium and potassium in the body, regulates metabolic processes, reduces the conductivity and excitability of the myocardium, eliminates the imbalance of electrolytes.
- "Digoxin". The basis of this drug is an extract of woolly foxglove. Improves heart function and lengthens diastole. Increases myocardial contractility, and, consequently, minute and stroke volume.
- Verapamil. Calcium channel blocker, which has antihypertensive, antiarrhythmic and antianginal effects. It affects both the myocardium and peripheral hemodynamics. Reduces myocardial oxygen demand, reduces its tone. If there is supraventricular arrhythmia, then it also has an antiarrhythmic effect.
These drugs should be taken 1 tablet 1-2 times a day. The course is usually 1-2 months.
Antiplatelet agents
These drugs are also used in the treatment of focal and diffuse cardiosclerosis. They do not allow aggregation (gluing) of platelets, and this is what leads to the formation of blood clots in the vessels. The best drugs in this category are:
- "Cardiomagnyl". This remedy not only inhibits platelet aggregation, it also has antipyretic, analgesic and anti-inflammatory effects.
- "Aspecard" and "Aspirin". These two drugs are analogues. They have the same effect as Cardiomagnyl. The antiplatelet effect is especially pronounced in platelets, since they cannot re-synthesize COX.
These drugs should be taken 1 tablet 1-2 times a day. All three of these drugs have a good thinning effect on the blood, and also improve blood circulation in the vessels and in the heart.

Other drugs
Continuing to talk about what it is - cardiosclerosis, and how to treat this disease, it is necessary to list other groups of medications prescribed to relieve symptoms.
With this pathology, nootropics are often prescribed, which have a specific effect on higher mental functions:
- "Fezam". It also has a vasodilating and antihypoxic effect. Improves blood flow, reduces the resistance of cerebral vessels and blood viscosity, improves the elasticity of erythrocyte membranes.
- "Piracetam". It has a positive effect on metabolic brain processes and integrative activity. Improves blood flow and connections between the hemispheres, stabilizes cerebral functions.
These drugs should be drunk on an ongoing basis, 1 tablet 2-3 times a day.
Medicines that improve heart rate are also often prescribed. These include Kordaron and Coronal.
With edema, which is one of the symptoms of the pathology in question, diuretics such as Veroshpiron and Furosemide help to cope. They should be taken 1 tablet 1 time per day for 2-3 weeks.
In addition to the above, with cardiosclerosis, you must definitely drink tonic. Namely, vitamins of group B. Their regular intake increases immunity and the body's defenses. This is necessary when he is weakened due to illness.
Food
One of the key points of effective treatment of cardiosclerosis is diet. You can not create a load on the internal organs with food. Therefore, it is important to follow these rules:
- Eat 5-6 times a day in small portions.
- Do not exceed the daily caloric intake of 2500-2700 kcal.
- Refuse s alt. Or at least keep it to a minimum.
- Cook food exclusively for a couple. Fried, stewed, baked, etc. are prohibited.
- Include a maximum of trace elements and vitamins in your daily diet. This means eating more fresh vegetables and fruits. Especially those with a high content of calcium and magnesium, which is necessary to improve the functioning of the cardiovascular system.
You will also need to give up these products:
- Cholesterol-rich food (sausage, fish, lard, meat).
- Alcohol.
- Some vegetables and herbs: radishes, onions, peas, parsley, beans, cabbage and garlic.
- Energy, strong tea, cocoa, coffee.
- Eggs and dairy products.
You still need to reduce the amount of fluid you drink. Per day - no more than 0.5 liters. What can be consumed with cardiosclerosis? In fact, it’s really possible to make a complete diet. And here's what:
- Fruits: cherries, apples, tangerines, kiwis, bananas and grapes. They can be used to make compotes, jellies, puddings, etc.
- Nuts.
- Vegetables other than those listed above.
- Rice and buckwheat porridge with low-fat milk.
- Fruit juices, especially carrot, apple and orange.
- Meat, poultry and fish with minimal fat (rare).
More detailed do's and don'tsmade by a doctor. He will discuss the topic of nutrition with the patient without fail.

Forecast
Much has been said above about the ICD codes for cardiosclerosis, the symptoms and causes of this disease, as well as how it should be treated. Finally, a few words about the forecast.
In this case, the change in the patient's condition, as well as his ability to work, depends on the severity of the pathology and the nature of its manifestation. If it is not burdened by circulatory and rhythm disorders, then the disease will proceed more favorably.
But if complications occur, the prognosis will worsen. Significantly complicates the course of the disease ventricular extrasystole, atrial fibrillation and circulatory failure. Also a significant danger is ventricular paroxysmal tachycardia, atrioventricular blockade and aneurysm, which was already mentioned earlier.
It is strongly recommended to carry out the prevention of pathology. If alarming symptoms appear, immediately consult a doctor, as well as promptly and actively treat atherosclerosis, coronary insufficiency and myocarditis.
People who have problems with the cardiovascular system or a tendency to develop them should undergo a scheduled examination by a cardiologist every six months.