- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
Ventricular flutter is a ventricular tachyarrhythmia that has a regular, fast rhythm (about 200-300 beats per minute). Most often, the condition may be accompanied by a decrease in blood pressure. Loss of consciousness, pallor, diffuse cyanosis of the skin, agonal breathing, convulsions, dilated pupils are not ruled out.
In addition, it can provoke sudden coronary death. Diagnosis of such a pathology is carried out on the basis of electrocardiographic studies and clinical data. Emergency care for ventricular flutter includes immediate defibrillation and cardiopulmonary resuscitation.

What is ventricular flutter?
A similar phenomenon is disorganized electrical activity of the myocardium, which is characterized by frequent and rhythmic contraction of the ventricles. The frequency of such contractions exceeds 200 beats per minute. It can also turn into fibrillation (flickering), whichwill present with frequent, up to 500 beats, but irregular and erratic ventricular activity.
In the cardiology department, experts classify fibrillation and flutter as a dangerous type of arrhythmia that can lead to inefficient hemodynamics. In addition, they are the most common causes of arrhythmic death. According to epidemiological data, fibrillation and flutter most often occur in individuals whose age ranges from 47 to 75 years. A characteristic feature is that in men they appear three times more often than in women. In 70-80% of cases, sudden death is caused by ventricular fibrillation.
Causes of pathology?
Ventricular flutter can occur against the background of various heart diseases, in the presence of a variety of extracardiac pathologies. Quite often, organic myocardial damage that develops against the background of IHD can be complicated by ventricular fibrillation and flutter. In addition, this pathology accompanies the following diseases:
- postinfarction cardiosclerosis;
- heart aneurysm;
- acute myocardial infarction;
- myocarditis;
- hypertrophic cardiomyopathy;
- dilated cardiomyopathy;
- Wolf-Parkinson-White syndrome;
- valvular heart disease (aortic stenosis, mitral valve prolapse).

Other reasons
Rarely, the development of this disorder may occur due to intoxicationcardiac glycosides, electrolyte imbalances, high blood levels of catecholamines, electrical injuries, chest injuries, cardiac concussions, hypoxia, acidosis, hypothermia. Also, ventricular tachycardia can be caused by some of the drugs, for example, sympathomimetics, barbiturates, narcotic analgesics, antiarrhythmics.
Another cause of flutter is cardiac surgery procedures. These include coronary angiography, electrical cardioversion, defibrillation in the cardiology department.
Pathogenesis of ventricular flutter
The development of such a disease is directly related to the re-entry mechanism, which has a circular nature of the circulation of the excitation wave passing through the ventricular myocardium. It causes the ventricles to contract frequently and rhythmically, and there is no diastolic interval. The re-entry loop can be located along the perimeter of the entire infarction zone, or the site of a ventricular aneurysm. The normal heart rate table by age will be presented below.
The main role in the pathogenesis of ventricular fibrillation is played by multiple random re-entry waves, which provoke the contraction of individual myocardial fibers while there are no ventricular contractions. This phenomenon is due to the electrophysiological heterogeneity of the myocardium: at the same time, different parts of the ventricles can be in the period of repolarization and in the period of depolarization.
What does it launch?
Ventricular fibrillation and flutter, as a rule, startsventricular and supraventricular extrasystoles. The re-entry mechanism can also initiate ventricular and atrial tachycardia, Wolff-Parkinson-White syndrome, atrial fibrillation, and then support them.

In the process of developing flutters and flickering, the stroke volume of the heart rapidly decreases, and then becomes zero. As a result, blood circulation stops instantly. Paroxysmal flutter and ventricular fibrillation are always accompanied by syncope, and a stable form of tachyarrhythmia entails first clinical and then biological death.
Classification of ventricular flutter
In the development process, heart diseases such as ventricular fibrillation and flutter go through four stages:
The first is the tachysystolic stage of ventricular flutter. The duration of this stage is a maximum of two seconds. It is characterized by frequent, coordinated heartbeats. On the ECG, this stage corresponds to 3-6 ventricular complexes with a sharp high-amplitude oscillation.
The second stage is convulsive ventricular tachyarrhythmia. Its duration is from 15 to 50 seconds. It is characterized by frequent, local contractions of the myocardium of an irregular nature. The ECG reflects this stage in the form of high-voltage waves of different magnitude and amplitude.
The third stage is the stage of ventricular fibrillation. The duration of this stage is 2-3 minutes. It is accompanied by multiple irregular contractions of individual zones of the myocardium,having different frequencies.
The fourth stage is atony. This stage develops approximately 2-5 minutes after the onset of ventricular fibrillation. The fourth stage is characterized by small, irregular waves of contractions, an increasing number of areas that have ceased to contract. On the ECG, they are reflected in the form of irregular waves, the amplitude of which gradually decreases.
Cardiologists distinguish between ventricular fibrillation and flutter according to the variant of their clinical development. So, there are permanent and paroxysmal forms. At the same time, fluttering of the second form can be recurrent in nature, that is, it can be repeated several times during the day.
Symptoms

Heart disease - ventricular fibrillation and flutter, in fact, correspond to clinical death. If flutter occurs, then for a short time, it is possible to maintain low cardiac output, consciousness and arterial hypotension. Rarely, ventricular flutter may result in spontaneous sinus-type rhythm recovery. Most often, such an unstable rhythm turns into ventricular fibrillation.
Flutter and ventricular fibrillation accompany the following symptoms:
- circulatory arrest;
- loss of consciousness;
- disappearance of the pulse on the femoral and carotid arteries;
- agonal breathing;
- sharp pallor;
- pupil dilation;
- diffuse cyanosis of the skin;
- lack of reaction to light;
- involuntarydefecation and urination;
- tonic spasms.

If these symptoms are observed and it is established that ventricular fibrillation and flutter have occurred, then the patient needs urgent medical attention. The CNS and other organs will be irreversibly damaged if normal heart rhythm is not restored within 4-5 minutes.
Complications
Death is the most unpleasant outcome of such deviations. The following complications may occur as a result of cardiopulmonary resuscitation:
- aspiration pneumonia;
- fractured ribs followed by a lung injury;
- hemothorax;
- pneumothorax;
- skin burns;
- various arrhythmias;
- hypoxic, anoxic, ischemic encephalopathy;
- myocardial dysfunction due to reperfusion syndrome.

Diagnosis of ventricular flutter
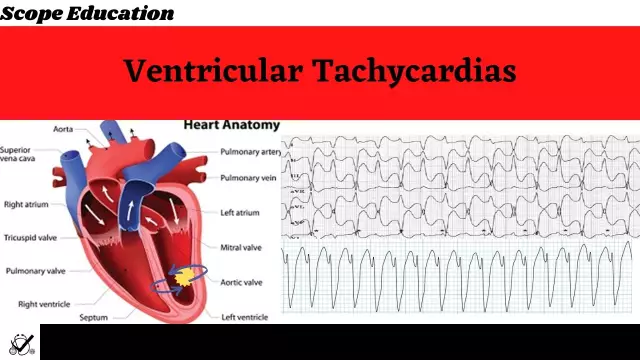
Ventricular fibrillation and flutter can be recognized and diagnosed using clinical and electrocardiographic data. If there is such a deviation, then on an electrocardiographic study it will be displayed in the form of regular, rhythmic waves that have almost the same shape and amplitude. They resemble a sinusoidal type curve with an oscillation frequency of 200-300 per minute. Also on the ECG there is no isoelectric line between the waves, P and T waves.
If there is ventricular fibrillation, there will bewaves with a heart rate (heart rate) of 300-400 oscillations per minute were recorded, which continuously change their duration, shape, direction and height. There is no isoelectric line between the waves.
Ventricular fibrillation and flutter must be differentiated from cardiac tamponade, massive PE, supraventricular arrhythmia, paroxysmal ventricular tachycardia.
The table of heart rate is normal by age is given below.

Ventricular flutter treatment
In the event of ventricular flutter or fibrillation, immediate resuscitation should be provided to restore sinus rhythm. Primary resuscitation should include precordial shock or artificial respiration in tandem with chest compressions. Specialized cardiopulmonary resuscitation includes mechanical ventilation and electrical defibrillation of the heart.
Simultaneously with resuscitation measures, solutions of atropine, adrenaline, sodium bicarbonate, procainamide, lidocaine, amiodarone, magnesium sulfate should be administered intravenously. In parallel with this, repeated electrodefibrillation is required. In this case, with each series, the energy should be increased from 200 to 400 J. If there is a recurrence of ventricular fibrillation and flutter, which occurs as a result of complete atrioventricular heart block, then it is necessary to resort to temporary stimulation of the heart ventricles with a rhythm that exceeds the frequency of their ownhesitation.
Special Instructions
If the patient does not recover spontaneous breathing, cardiac activity, consciousness within 20 minutes, there is no reaction to the light of the pupils, then resuscitation measures must be stopped. If the resuscitation was successful, then the patient is transferred to the ICU for further observation. Subsequently, the attending cardiologist decides whether it is necessary to implant an cardioverter-defibrillator or a dual-chamber pacemaker.