- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2024-01-17 01:02.
- Last modified 2025-06-01 06:18.
The uterus is the reproductive unpaired internal organ of the female. It is made up of plexuses of smooth muscle fibers. The uterus is located in the middle part of the small pelvis. It is very mobile, therefore, relative to other organs, it can be in different positions. Together with the ovaries, it makes up the reproductive system of the female body.
General structure of the uterus
This internal muscular organ of the reproductive system is pear-shaped, which is flattened front and back. In the upper part of the uterus on the sides there are branches - the fallopian tubes, which pass into the ovaries. Behind is the rectum and in front is the bladder.
The anatomy of the uterus is as follows. The muscular organ consists of several parts:
- The bottom is the upper part, which has a convex shape and is located above the line of origin of the fallopian tubes.
- The body into which the bottom smoothly passes. It has a conical shape. Tapers down and forms an isthmus. This is the cavity leading to the cervix.
- Cervix - consists of the isthmus, cervical canal and vaginal part.
The size and weight of the uterus are individual. The average values of her weight in girls and nulliparous women reach 40-50 g.

The anatomy of the cervix, which is a barrier between the internal cavity and the external environment, is designed so that it protrudes into the anterior part of the vaginal fornix. At the same time, her posterior fornix remains deep, and the anterior one, on the contrary.
Where is the uterus?
The organ is located in the small pelvis between the rectum and the bladder. The uterus is a very mobile organ, which, in addition, has individual characteristics and shape pathologies. Its location is significantly affected by the condition and size of neighboring organs. The normal anatomy of the uterus in the characteristics of the place occupied in the small pelvis is such that its longitudinal axis should be oriented along the axis of the pelvis. Its bottom is tilted forward. When filling the bladder, it moves back a little, when emptying, it returns to its original position.

The peritoneum covers most of the uterus, except for the lower part of the cervix, forming a deep pocket. It extends from the bottom, goes to the front and reaches the neck. The back part reaches the wall of the vagina and then passes to the anterior wall of the rectum. This place is called Douglas space (depression).
Uterine anatomy: photo and wall structure
Three-layer body. It consists of: perimetrium, myometrium and endometrium. The surface of the uterine wall is covered by the serous membrane of the peritoneum - the initial layer. At the next - middle level - tissues thicken and have a more complex structure. Plexussmooth muscle fibers and elastic connective structures form bundles that divide the myometrium into three inner layers: inner and outer oblique, circular. The latter is also called the average circular. This name he received in connection with the structure. The most obvious is that it is the middle layer of the myometrium. The term "circular" is justified by the rich system of lymphatic and blood vessels, the number of which increases significantly as it approaches the cervix.

Bypassing the submucosa, the wall of the uterus after the myometrium passes into the endometrium - the mucous membrane. This is the inner layer, reaching a thickness of 3 mm. It has a longitudinal fold in the anterior and posterior region of the cervical canal, from which small palm-shaped branches extend at an acute angle to the right and left. The rest of the endometrium is smooth. The presence of folds protects the uterine cavity from the penetration of unfavorable contents of the vagina for the internal organ. The endometrium of the uterus is prismatic, on its surface are the uterine tubular glands with vitreous mucus. The alkaline reaction they give keeps the sperm viable. During the period of ovulation, secretion increases and substances enter the cervical canal.
Uterine ligaments: anatomy, purpose
In the normal state of the female body, the uterus, ovaries and other adjacent organs are supported by a ligamentous apparatus, which is formed by smooth muscle structures. The functioning of the internal reproductive organs largely depends on the conditionmuscles and fascia of the pelvic floor. The ligamentous apparatus consists of a suspension, fixation and support apparatus. The combination of the properties of each of them ensures the normal physiological position of the uterus among other organs and the necessary mobility.
| Apparatus | Performed functions | The ligaments that form the apparatus |
| Hanging | Connects uterus to pelvic wall | Paired wide uteruses |
|
Sustaining ligaments of the ovary |
||
| Ovary's own ligaments | ||
| Round ligaments of uterus | ||
| Fixing | Fixes the position of the body, stretches during pregnancy, providing the necessary mobility | Main uterine ligament |
| Vesicouterine ligaments | ||
| Uterosacral ligaments | ||
| Supportive | Forms the pelvic floor, which is a support for the internal organs of the genitourinary system | Muscles and fascia of the perineum (outer, middle, inner layer) |
The anatomy of the uterus and appendages, as well as other organs of the female reproductive system, consists of developed muscle tissue and fascia, which play a significant role in the normal functioning of the entire reproductivesystem.
Characteristics of the suspension device
The suspension apparatus is made up of paired ligaments of the uterus, thanks to which it is “attached” at a certain distance to the walls of the small pelvis. The wide uterine ligament is a fold of the peritoneum of the transverse type. It covers the body of the uterus and the fallopian tubes on both sides. For the latter, the ligament structure is an integral part of the serous cover and the mesentery. At the side walls of the pelvis, it passes into the parietal peritoneum. The supporting ligament departs from each ovary, has a wide shape. Characterized by durability. Inside it passes the uterine artery.

The own ligaments of each of the ovaries originate at the uterine fundus from the back side below the branch of the fallopian tubes and reach the ovaries. The uterine arteries and veins pass inside them, so the structures are quite dense and strong.
One of the longest suspension elements is the round ligament of the uterus. Its anatomy is as follows: the ligament has the form of a cord up to 12 cm long. It originates in one of the corners of the uterus and passes under the front sheet of the broad ligament to the internal opening of the groin. After that, the ligaments branch into numerous structures in the fiber of the pubis and labia majora, forming a spindle. It is thanks to the round ligaments of the uterus that it has a physiological inclination anteriorly.
Structure and location of fixing ligaments
The anatomy of the uterus should have assumed its natural purpose - bearing and giving birth to offspring. This process is inevitably accompaniedactive contraction, growth and movement of the reproductive organ. In this connection, it is necessary not only to fix the correct position of the uterus in the abdominal cavity, but also to provide it with the necessary mobility. For just such purposes, fixing structures arose.
The main ligament of the uterus consists of plexuses of smooth muscle fibers and connective tissue, located radially to each other. The plexus surrounds the cervix in the region of the internal os. The ligament gradually passes into the pelvic fascia, thereby fixing the organ to the position of the pelvic floor. The vesicouterine and pubic ligamentous structures originate at the bottom of the front of the uterus and attach to the bladder and pubis, respectively.
The sacro-uterine ligament is formed by fibrous fibers and smooth muscles. It departs from the back of the neck, envelops the rectum on the sides and connects to the fascia of the pelvis at the sacrum. When standing, they are vertical and support the cervix.
Support apparatus: muscles and fascia
The anatomy of the uterus implies the concept of "pelvic floor". This is a set of muscles and fascia of the perineum, which make it up and perform the function that supports the internal genital organs of a woman. The pelvic floor consists of an outer, middle and inner layer. The composition and characteristics of the elements included in each of them are given in the table:
| Layer | Muscles | Characteristic |
| Outdoor | Ischial-cavernous | Steam room, located from the buttocks to the clitoris |
| Bulbous Spongy | Steam room, wraps around the entrance to the vagina, thereby allowing it to contract | |
| Outdoor | Squeezes the "ring" of the anus, surrounds the entire lower rectum | |
| Surface transverse | Weakly developed pair muscle. It comes from the ischial tuberosity from the inner surface and is attached to the tendon of the perineum, connecting with the muscle of the same name, coming from the back side | |
| Medium (urogenital diaphragm) | m. sphincter urethrae externum | Constricts the urethra |
| Deep transverse | Steam room, located between the symphysis, pubis and ischium. | |
| Internal (pelvic diaphragm) | Pubococcygeal | Pair branches m. levator ani, which elevates the anus. Well developed. |
| Iliococcygeal | ||
| Ischiococcygeal |
The normal anatomy of the uterus and appendages is ensured precisely by the pelvic floor, which is the main support of the internal organs of the genitourinary system. The correct arrangement of organs is the key to their he althy functioning. Damage and significant weakening of the pelvic floor muscles threatens to prolapseand even organ prolapse.
Structure of the ovaries and appendages
Anatomy of the uterus, ovaries are reproductive organs connected to each other by means of the fallopian tubes. The ovaries are the sex glands located on either side of the uterus. Inside them, during the menstrual cycle, eggs mature, which then enter the uterine cavity through the fallopian tubes.

The ovaries are fixed with a suspensory ligament and mesentery. Unlike the uterus, they are not covered by the peritoneum. The structure of the ovary is based on the medulla and cortex. The latter contains mature follicles. On the inside, a granular layer adjoins the wall, in which the egg cell lies. It is surrounded by a radiant crown and a transparent zone.
During ovulation, the follicle approaches the outer layer of the ovary and bursts. This releases the egg and enters the uterus through the fallopian tube. The bursting follicle replaces the corpus luteum, which gradually disappears in the absence of pregnancy. If fertilization occurs, the corpus luteum continues to exist for the entire period to perform intrasecretory functions.
The surface of the ovaries is covered with a white membrane formed by connective tissue. Each ovary is surrounded by appendages having a convoluted shape and consisting of longitudinal and transverse tributaries. They are considered vestigial formations.
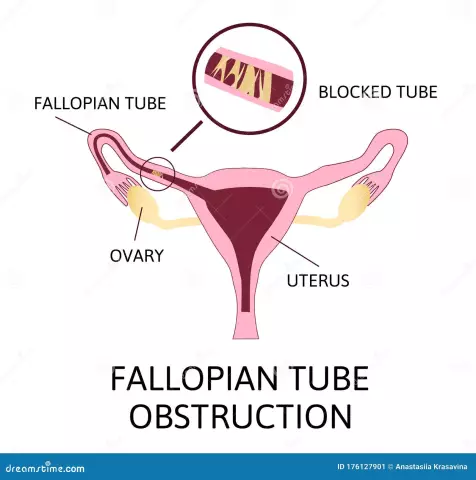
Falling tubes
Paired organ, with the help of which the egg from the abdominal cavity enters the uterus. Fallopian tubes are oval shaped ductspass through the upper part of the broad ligament of the uterus. Their length can be up to 13 centimeters, and a diameter of 3 mm. Transportation of the egg is carried out using the uterine and abdominal openings, the name of which corresponds to the cavities into which it exits.
Fallopian tubes consist of:
- uterine part - located in the thickness of the uterus;
- isthmus - the narrowest part with thick walls;
- ampoules;
- funnel - through their lumen, the egg enters the fallopian tube;
- fringes - they direct the egg to the funnel.
Inside the tube is lined with a mucous membrane with ciliated epithelium and longitudinal folds, the number of which increases as it approaches the abdominal opening. From the outside, the fallopian tubes are covered with a serous membrane.
The structure of the circulatory system
The blood supply to the reproductive organ is due to the uterine artery, which is a branch of the internal iliac artery. The anatomy of the uterus and fallopian tubes involves the outflow of blood from two sides, so the artery has two branches. Each of them is located along the broad ligament, then dividing into smaller vessels that go to the anterior and posterior surfaces of the organ. Near the uterine fundus, the vessel branches again to provide blood flow to the fallopian tubes and ovaries.

Uterine veins are formed from the venous plexus, where venous blood flows. From here, the veins originate, which then flow into the internal iliac, ovarian veins and plexuses of the rectum. Venous outflow after the uterine and ovarian veins passes to the iliac and inferior vena cava.
Lymph outflow from the internal genital organs
Lymph nodes, to which lymph is sent from the body and cervix - iliac, sacral and inguinal. They are located at the place of passage of the iliac arteries and on the anterior part of the sacrum along the round ligament. Lymphatic vessels located at the bottom of the uterus reach the lymph nodes of the lower back and inguinal region. The common plexus of lymphatic vessels from the internal genital organs and rectum is located in the space of Douglas.
Innervation of the uterus and other female reproductive organs
The internal genital organs are innervated by the sympathetic and parasympathetic autonomic nervous system. The nerves going to the uterus are usually sympathetic. On their way, spinal fibers and structures of the sacral nerve plexus join. Contractions of the body of the uterus are regulated by the nerves of the superior hypogastric plexus. The uterus itself is innervated by branches of the uterovaginal plexus. The cervix usually receives impulses from the parasympathetic nerves. The ovaries, fallopian tubes, and adnexa are innervated by both the uterovaginal and ovarian plexuses.
Functional changes during the monthly cycle
The wall of the uterus is subject to changes both during pregnancy and throughout the menstrual cycle. The sexual cycle in the female body is characterized by a set of ongoing processes in the ovaries and uterine mucosa under the influence of hormones. It is divided into 3 stages:menstrual, postmenstrual and premenstrual.
Desquamation (menstrual phase) occurs if fertilization does not occur during ovulation. The uterus, a structure whose anatomy consists of several layers, begins to shed the mucous membrane. Together with her, the dead egg comes out.

After rejection of the functional layer, the uterus is covered with only a thin basal mucosa. Postmenstrual recovery begins. In the ovary, the corpus luteum is re-produced and a period of active secretory activity of the ovaries begins. The mucous membrane thickens again, the uterus is preparing to receive a fertilized egg.
The cycle continues uninterrupted until fertilization occurs. When the embryo implants in the uterine cavity, pregnancy begins. Every week it increases in size, reaching 20 or more centimeters in length. The birth process is accompanied by active contractions of the uterus, which contributes to the oppression of the fetus from the cavity and the return of its size to prenatal.
The uterus, ovaries, fallopian tubes and adnexa together form the complex female reproductive organ system. Thanks to the pelvic floor and mesentery, the organs are securely fixed in the abdominal cavity and protected from excessive displacement and prolapse. The blood flow is provided by a large uterine artery, and several nerve bundles innervate the organ.