- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
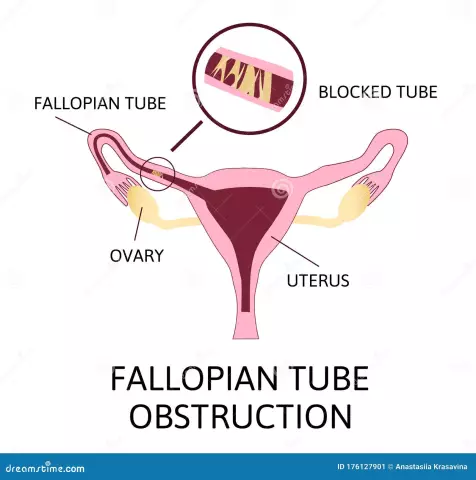
Almost every woman wants to hear the cherished "mother" from her son or daughter. However, for a number of reasons this is not possible. And one of these is the poor patency of the fallopian tubes (which are popularly referred to as the oviducts), which can lead to undesirable consequences such as tubal pregnancy or infertility. To determine the exact causes of this phenomenon, a woman is sent by a gynecologist for a special examination.
What it is, what it is for and how the problem can be fixed - read in this article. But first, let's consider the probable causes of this kind of pathology.
What could be the reasons?
As you know, under normal conditions, a mature egg leaves the ovary and begins its journey through the fallopian tube, with the help of cilia that cover the entire inner surface of the epithelium. Here she hopes to meet with the male germ cell, resulting infertilization.

Cells begin to divide, an embryo is formed, which, with good patency of the fallopian tubes, reaches the uterine cavity for some period of time, where it is fixed on the wall of the endometrium. But under certain circumstances, the patency of the fallopian tubes can be changed, and then the normal course of pregnancy is impossible.
The female reproductive organ, called the uterus, is the only cavity where the full development of the fetus is possible. The possibility of successful conception and bearing of a child fully depends on the he alth of this organ and the condition of the fallopian tubes themselves.
According to experts in the field of infertility research, 30-40% of the total number of reported cases is associated with obstruction of the fallopian tubes. The reasons for the appearance of this pathology, prompting to check the patency of the fallopian tubes, may be different. First of all, this:
- The course of inflammation caused by the active activity of trapped bacteria.
- Sexually transmitted diseases like gonorrhea, chlamydia, trichomoniasis, genital herpes and a number of other infections.
- Gynecological operations, including possible complications after them.
- Performing abortions.
- Surgical intervention to treat diseases of the abdominal cavity and small pelvis - appendicitis, peritonitis.
- Presence of diseases of the reproductive system - salpingitis, sactosalpinx, endometriosis, uterine fibroids.
Another reason for deviations in the structure of the fallopian tubes, including their complete or partial absence, is a congenital feature of the body. In addition, another reason to check the patency of the fallopian tubes can be various strong stressful situations or hormonal imbalances, only this happens extremely rarely.
Effective diagnostic techniques
To make a diagnosis of infertility, which is disappointing for most women, or, conversely, to refute it, specialists need to figure out why this phenomenon is caused. Then the appropriate treatment will be prescribed.

As medical practice shows, many women learn about the presence of any inflammatory process randomly during the diagnosis. In this regard, you should not refuse planned gynecological examinations, which must be done every 6 months.
How do they diagnose the patency of the fallopian tubes and what is the name of the procedure? For this, different methods are used, each of which has its own advantages and disadvantages. The methods proven over the years are painful and, in addition, require long-term clinical studies. In addition, they are performed only with the use of general anesthesia. As for modern techniques, they are relatively painless, general anesthesia is not required in this case.
The following diagnostics are currently available:
- Hydrosonography.
- Laparoscopy.
- Hysterosalpingography.
In order for a woman to choose the most appropriate type of examination, she needs to consult a gynecologist in order to obtain a gynecological history. And depending on this information, the doctor will advise the best diagnostic option.
So-called testimony
There are a number of characteristic signs, the presence of which allows a woman to think about the need to study the patency of the fallopian tubes. These include the following manifestations:
- The menstrual cycle has become irregular or completely stopped.
- Expected pregnancy does not occur for more than 6 months.
- Inflammatory processes of the appendages are regular or chronic.
- Presence of infectious diseases that are sexually transmitted.
- Pain in the lower abdomen.
All these signs clearly indicate that unwanted processes are occurring in the female body. Therefore, it is better to play it safe once again by visiting a doctor. In addition, it is not possible to check the condition of the fallopian tubes on your own, since this simply cannot be done without special equipment.
Ultrasound of the patency of the fallopian tubes
The patency of the fallopian tubes can be checked without resorting to a high dose of x-rays. An ultrasound machine comes into play, in which the reliability of the study is up to 90%. Moreover, in our time several dimensions are available: these are 2D, 3D and even 4D. This technique, in addition to the name hydrosonography, also hasone name - echosalpingography (echohydrotubation).

The method is easy to implement, the study is carried out directly in the office. To visually confirm or refute the diagnosis, the examination is carried out in two ways:
- Through the abdominal wall.
- Transvaginally - through a special probe that is inserted into the vagina.
In the course of an ultrasound of the patency of the fallopian tubes, everything depends on the qualifications of the operator who operates the device, and his ability to correctly interpret the images obtained. The procedure is performed in the period from the 5th to the 20th day of the menstrual cycle, but experts still recommend applying no later than the 8th-11th day, since during this period the moment of ovulation is closest. In this case, the likelihood of spasms is minimal, it is easier to inject the concentrate.
During the diagnosis, a woman may experience discomfort, which is a disadvantage of this type of study. In addition, contraceptive measures must be observed before the procedure.
Laparoscopy
Many women are not interested in the name of the tubal patency procedure, but in how it is carried out. Specifically, this diagnosis refers to the surgical method, which is characterized by minimal damage to the skin. During the procedure, it is possible not only to establish the fact of obstruction, but also to eliminate the cause of the "blockage".
Stationary conditions are required for this kind of operation. On theseveral small incisions are made on the surface of the skin of the abdominal wall. Subsequently, an optical system equipped with micro-illuminators and a manipulator is introduced through them. In order to improve visual observation, the abdominal cavity is filled with carbon dioxide.
To assess the degree of patency of the fallopian tubes, an aqueous solution of methylene blue is injected into the uterus, and a special video camera allows you to see if this substance passes through them. Moreover, diagnostics are carried out, as they say, in real time.

Since such a diagnosis requires surgical intervention, albeit to a small extent, a recovery period is necessary after it. Fortunately, in this case, it passes quickly and usually takes two to three days, no more.
Among all the available diagnostic methods, laparoscopy is the most accurate technique, in which it is not inferior to either hysterosalpingography or ultrasound. In addition, the risk of adhesion formation is the lowest.
HHA
Hysterosalpingography of the fallopian tubes is carried out by radiography. In this case, you can:
- Determine the degree of patency of the pipes.
- Detect the presence of deformation of the reproductive organ or appendages.
- Assess the condition of the endometrium.
- Detect any pathological changes.
Research is best done before ovulation in the follicular phase of the menstrual cycle. At the same time, there is no need for anesthesia, and the procedure itself is performed on an outpatient basis.
Everything is done as follows. A special contrast agent is introduced into the cavity of the genital organ through the cervical canal by means of a catheter. Then x-rays are taken at the initial and final stages of the study. And they evaluate the results of the HSG of the fallopian tubes.
The first image allows you to evaluate the shape of the uterine cavity, determine the clarity of the contours, as well as identify possible pathological changes in the tubes, including the degree of their patency. Thanks to the second picture, you can see the spread of the contrast agent in the pelvic area, if, of course, it goes there.
If we compare such diagnostics with laparoscopy, it is less accurate (only 80%). At the same time, it is well tolerated by women, despite the unpleasantness of the whole procedure. It is very important that there are no inflammatory processes. Let us dwell in more detail on this type of diagnostics and consider many features.
Tubal HSG preparation
If a woman has been prescribed hysterosalpingography (or HSG, in a simple way), she needs to properly prepare for this procedure. For some reason, many doctors forget to warn patients that the procedure is quite painful and can cause a lot of discomfort. In this connection, good moral preparation is needed.

Before the study, a woman should have fresh urine and blood tests on her hands. You may also need a gynecological smear and scrapings of the cervix and cervical canal. In addition, notit is excluded that tests for the presence of STDs (HIV, TORCH infection) will be needed.
You must also fulfill a number of necessary requirements:
- Abstain from sexual contact for a day or two before the HSG procedure.
- Do not douche for a week and refuse any kind of intimate hygiene products.
- Also, do not use any kind of medicine like vaginal suppositories, tablets, sprays for a week. Unless there is a need for a hysterosalpingogram on the advice of a physician.
Another question that may arise regarding the HSG of the fallopian tubes: on what day of the cycle is such a procedure performed? As a rule, this is the period when menstruation ends, while ovulation has not yet occurred. It is during this period of time that the condition of the endometrium makes it possible to detect the presence of endometriosis.
On the day of the procedure, a woman needs to empty her intestines with an enema or laxative. And just before the start of the GHA, it is worth visiting the restroom. It will not hurt to take a sedative, which will allow uterine contractions not to interfere with the procedure itself.
When the hysterosalpingography is completed, within a few days (usually 1-3 days), contrast agent and blood may leak out. Therefore, you should take tampons, pads, or use disposable underwear with you to the hospital.
Contraindications for HSG
The main medical indication for the procedure is the provisional diagnosis of infertility. It is very important to carry outadditional examinations before the HSG of the fallopian tubes, blood or urine tests, as there are contraindications for the procedure, which include:
- Pregnancy fact.
- Allergic predisposition of the body to the contrast agent.
- The presence of diseases of the reproductive system of an infectious nature.
It is for this reason that before carrying out the HSG procedure, analyzes and some other studies are needed.
Consequences and complications
As a rule, such a diagnostic procedure as hysterosalpingography is safe for a woman, and after it there are no serious consequences or complications. However, it is impossible to completely exclude any side effects. We are talking about an allergic reaction to a contrast agent, which is extremely rare. In addition, allergic manifestations can occur in the presence of bronchial asthma.

Complications after tubal HSG can be early or late. In addition to allergies, early complications include:
- Vascular reflux, when a contrast agent enters the capillaries or veins of the reproductive organ.
- Lymphatic reflux: Fluid is already entering the lymphatic network of the uterus.
- Perforation of the uterine wall is a penetrating injury caused by careless actions of medical personnel.
- Pipe burst if too much pressure is applied.
Long-term complications include inflammatory reactions that occur due to infection duringthe time of the procedure, again due to careless actions on the part of the medical staff.
What the GHA results show
According to the pictures taken, the specialist can proceed to their analysis. The result is evaluated by the degree of distribution of the contrast agent in the internal organs of the female body. If it is noticeable that it has penetrated into the fallopian tube from the uterus, and from there into the circulatory system, then this indicates their good patency.
In addition to the fact that in the course of this diagnosis one can judge the degree of patency of the oviducts, one can also detect a number of pathological changes that directly affect the he alth of the female body and serve as a serious obstacle to conceiving a child. These include:
- polyps;
- benign neoplasms in the form of uterine fibroids;
- spikes;
- hydrosalpinx and a number of other cases.
Despite the fact that the determination of the degree of patency of the fallopian tubes by means of hysterosalpingography has been used in medicine for many years, the results are not always very accurate. And this is even with the right procedure. The accuracy of the results is evaluated by two criteria: sensitivity and specificity.

Where can I take the GHA?
Currently, to diagnose the condition of the fallopian tubes, women can go to public or private clinics, where there is usually a wide range of services provided. Several decades agoconfirmation of infertility for a woman was a terrible diagnosis, which simply put an end to the possibility of becoming pregnant. But thanks to the achievements of modern medicine, restoring the functionality of the fallopian tubes is no longer a problem.
In addition to the question of where the HSG of the fallopian tubes is done, every woman is also interested in the price of the procedure. It depends on the type of diagnosis, the degree of accuracy of the results obtained, as well as the possible risks of complications.