- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-06-01 06:18.
Panniculitis is a progressive process of inflammation of the subcutaneous tissue, which destroys fat cells, they are replaced by connective tissue, nodes, infiltrates and plaques are formed. With the visceral type of the disease, the fat cells of the kidneys, liver, pancreas, fatty tissue of the omentum or the area behind the peritoneum are affected. In about 50% of cases, the pathology takes an idiopathic form, which is mainly observed in women 20-50 years old. The other 50% is secondary panniculitis, which develops against the background of systemic and skin diseases, immunological disorders, and the influence of various provoking factors (cold, certain drugs). The formation of panniculitis is based on a defect in lipid peroxidation.

Reasons for appearance
This inflammation of the subcutaneous tissue can be caused by various bacteria (mainly staphylococci and streptococci). In most cases, it develops inlower limbs. The disease can appear after a fungal infection, injury, dermatitis, ulcer formation. The most vulnerable areas of the skin are those that have excess fluid (for example, with swelling). Also, panniculitis may appear in the area of scars after operations.
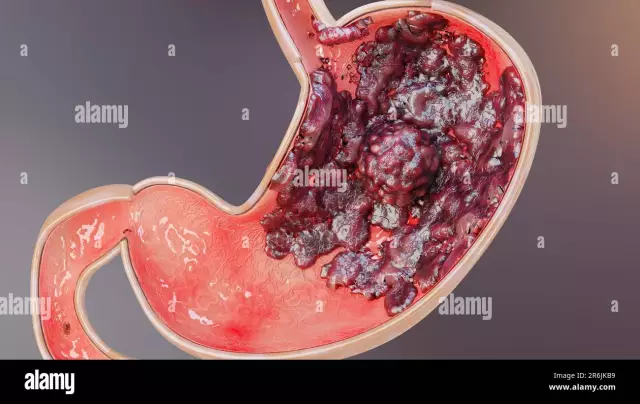
In the photo, inflammation of the subcutaneous tissue is difficult to notice.
Symptoms of panniculitis
The main manifestation of spontaneous panniculitis is nodular formations located at different depths in the subcutaneous fat. They usually appear on the legs and arms, rarely on the abdomen, chest and face.
After nodular destruction, atrophied foci of fatty tissue remain, having the form of round areas of skin retraction. The nodular variant is distinguished by the appearance of typical nodes in the tissue under the skin ranging in size from three millimeters to five centimeters.
Integuments of the skin over the nodes can be stained in the usual color or be bright pink. With a plaque type of inflammation of the subcutaneous adipose tissue, separate nodular accumulations appear, which coalesce and form tuberous conglomerates.
Over such formations, the skin can be burgundy-bluish, burgundy or pink. In some cases, nodular accumulations extend completely to the tissue of the shoulder, lower leg or thigh, squeezing the vascular and nerve bundles. Because of this, obvious soreness appears, lymphostasis develops, limbs swell.
The infiltrative type of the disease passes with the melting of nodes and their conglomerates. In the area of the node or plaque, the skin is bright red or burgundy. Then a fluctuation occurs, whichcharacteristic of abscesses and phlegmon, however, when the nodes are opened, a yellow oily mass is released, and not pus. A long non-healing ulcer will remain in place of the opened node.
With a mixed type of panniculitis, the nodular form turns into a plaque, then into an infiltrative one. This option is noted in rare cases. At the onset of the disease, there may be fever, muscle and joint pain, nausea, headaches, and general weakness. With the visceral type of the disease, systemic inflammation of fatty tissue occurs throughout the human body with the formation of specific nodes in the fiber behind the peritoneum and omentum, pancreatitis, hepatitis and nephritis. Panniculitis can last from two to three weeks up to several years.

Diagnostic Methods
Inflammation of the subcutaneous tissue, or panniculitis, is diagnosed at a joint examination by a dermatologist and a nephrologist, a rheumatologist, a gastroenterologist. Urine and blood tests, the study of pancreatin enzymes, Reberg's test, and liver tests are used. The definition of nodes in visceral type panniculitis occurs due to ultrasound examination of the abdominal organs and kidneys. Blood culture for sterility helps to exclude the septic orientation of the disease. An accurate diagnosis is made after obtaining a biopsy of the formation with histological analysis.
Classification
There are primary, spontaneous and secondary forms of inflammation of the subcutaneous tissue. Secondary panniculitis are:
- immunologic panniculitis -occurs frequently in systemic vasculitis;
- lupus-panniculitis (lupus) - with a deep lesion of systemic lupus erythematosus;
- enzymatic panniculitis - associated with the influence of pancreatic enzymes;
- proliferative cell panniculitis - with lymphoma, histiocytosis, leukemia, etc.;
- cold panniculitis is a local form that develops as a reaction to exposure to cold;
- steroid panniculitis - appears in children after completion of corticosteroid treatment;
- artificial panniculitis - caused by drug administration;
- crystalline panniculitis - appears in renal failure, gout due to the deposition of calcifications, urates in the fiber;
- hereditary panniculitis, which is caused by a lack of α1-antitrypsin.
Nodular, plaque and infiltrative types of the disease are distinguished by the shape of the nodes.

Patient actions
If the first signs of panniculitis appear, you need to see a doctor. Among other things, you should seek medical attention if you develop new symptoms (persistent fever, drowsiness, extreme fatigue, blistering, and increased redness).
Features of treatment
The method of treating inflammation of the subcutaneous tissue is determined by its course and form. In chronic nodular panniculitis, anti-inflammatory non-steroidal agents (Ibuprofen, Diclofenac sodium), antioxidants (vitamins E and C) are used; chip off nodal formationsglucocorticoids. Physiotherapeutic procedures are also effective: hydrocortisone phonophoresis, ultrasound, UHF, laser therapy, ozocerite, magnetotherapy.
In the plaque and infiltrative type, the subacute course of the disease is characterized by the use of glucocorticosteroids (Hydrocortisone and Prednisolone) and cytostatics (Methotrexate). Secondary forms of the disease are treated with therapy against the background of vasculitis, gout, pancreatitis and systemic lupus erythematosus.

From panniculitis, a preventive measure is the timely diagnosis and treatment of primary pathologies - bacterial and fungal infections, lack of vitamin E.
How does inflammation of the subcutaneous tissue on the legs manifest?
Cellulite
Cellulite, or gynoid lipodystrophy, is caused by structural changes in adipose tissue, often leading to severe deterioration of blood microcirculation and lymph stagnation. Not all experts consider cellulite a disease, but they insist that it can be called a cosmetic defect.
Such inflammation of the subcutaneous fat is shown in the photo.

Mostly cellulite occurs in women as a result of hormonal disruptions that occur periodically: adolescence, pregnancy. In some cases, its appearance can provoke the use of hormonal contraceptives. Of great importance is the factor of heredity and the specifics of the diet.
How to get rid of?
Tissue lipodystrophy under the skin is treatednecessarily complex. To achieve success, you need to eat right, drink multivitamins, antioxidants. A very important part of the treatment is sports activities and active breathing.

Doctors recommend a course of procedures to improve blood and lymph circulation - bioresonance stimulation, massage, pressure and magnetotherapy. Fat cells become smaller after mesotherapy, ultrasound, electrolyolysis and ultraphonophoresis. They use special anti-cellulite creams.