- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
A common heart rhythm disorder is called supraventricular tachycardia. As a rule, it is presented with recurring episodes of an increase in the frequency of the beat and heaviness in the region of the organ. Although SVT is not usually life-threatening, many patients suffer from recurring symptoms that have a significant impact on their quality of life. The indeterminate and sporadic nature of tachycardia episodes can be a significant concern for many individuals.
Suddenly rapid heartbeat characterizes SVT, and in most patients the diagnosis can only be made with a high degree of certainty from the medical history. Repeated attempts at electrocardiographic studies may prove futile.

The incidence of SVT is about 35 cases per 100,000 population per year, the prevalence is 2.25 per 1,000 inhabitants. Usually manifests as a recurring paroxysm of supraventricular tachycardia, the symptoms of which lead to an acute course of the disease. The main types of SVT are: Wolff-Parkinson-White syndrome, supraventricular or supraventricular extrasystole,atrioventricular junctional reentry tachycardia.
How does the heart work?
The vital organ consists of four chambers - two atria and two ventricles. Each heartbeat begins with tiny electrical impulses produced in the sinoatrial node. It is the pacemaker at the top of the right atrium. An electrical impulse travels through the heart muscle, causing it to work. Initially, it moves through the atria, passing into the atrioventricular node, which acts as a distributor. It then passes through the atrioventricular bundle, which acts as a conductor that delivers impulses to the ventricles. In turn, the ventricles begin to supply blood to the arteries.
What is supraventricular tachycardia and what causes it?
This disease means a rapid heartbeat from above the ventricle, not controlled by the sinoatrial node. Another part of the heart blocks the electrical impulses in the pacemaker. The source begins above the ventricles, spreading to them. In most cases, SVT begins in early adulthood. Supraventricular tachycardias in children are also common. However, it can occur at any age. This is a rare disease, but the exact number of people affected is unknown.

Supraventricular supraventricular tachycardia is caused by:
- Drugs. These include some inhalers, herbal supplements, and cold remedies.
- Using bigamounts of caffeine and alcohol.
- Stress or emotional upset.
- Smoking.
Atrioventricular and atrial type of SVT. Wolff-Parkinson-White Syndrome
AVNRT is the most common type of supraventricular tachycardia. Most often observed in people over 20 years old and in women over 30. Occurs when an electrical impulse closes in the center of the heart. It often manifests itself in absolutely he althy individuals. Instead of the subsequent normal activation and pulse, the sinotrial node releases additional current around this short circuit. This means that the heart rate will increase rapidly and then all the symptoms of SVT will appear.
Atrial tachycardia is a less common type. It occurs on a small area of tissue, anywhere in both atria of the heart. In most cases, the causes are unknown. However, it can appear in areas where a myocardial infarction has previously occurred, or there are problems with the heart valve. Wolff-Parkinson-White syndrome develops very quickly. There are symptoms of dizziness, loss of consciousness is possible. Sudden death is a complication of this condition, but it is extremely rare.
Clinical manifestations
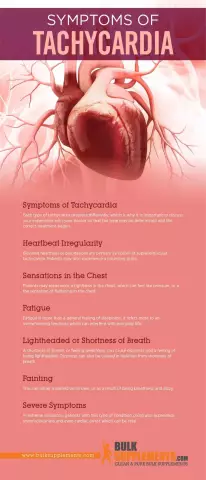
Symptoms of supraventricular tachycardia can last for seconds, minutes or even hours.
The following manifestations are possible:
- The pulse becomes 140-200 beats per minute.
- Sometimes it can be faster.
- Heart pounding sensation.
- Dizziness, difficultbreath.

SVT usually starts suddenly, for no apparent reason. Paroxysmal supraventricular tachycardia is manifested by a pulsation in the neck or head, and may also be accompanied by chest discomfort (unaccustomed pain), shortness of breath, anxiety. Often, blood pressure drops due to a fast heart rate, especially if it persists for several hours. In some cases, this leads to fainting or collapse.
The severity of symptoms varies greatly, depending on the function and frequency of contractions, the duration of supraventricular tachycardia, concomitant heart diseases. The individual perception of the patient also matters. Myocardial ischemia may occur.
Disease diagnosis
There are several ways to diagnose a disease such as supraventricular tachycardia: ECG, echocardiogram, testing the heart with exercises. In many cases, the test results are usually normal.
An electrocardiograph examines the rhythm and electrical activity of an organ. This is a painless procedure and takes a few minutes. If PVT occurs during an ECG, the machine can confirm the diagnosis and thereby rule out other causes of rapid heartbeat.

Since it is not always possible to diagnose the presence of a disease in a hospital setting, the patient is advised to try to identify the disease withusing a portable electrocardiograph. It will record in memory all the processes that occur with the heart within 24 hours. Swimming is prohibited during the procedure.
You may need to use an echocardiogram. It is necessary to assess cardiac structure and function, but the results are usually within the normal range. You will also need to perform some exercises necessary to determine when exactly the tachycardia occurs (during exercise or at rest). Patients may complain of chest pain during SVT. These symptoms do not require a stress test or angiography. The decision on further testing should be based on the patient's history and the presence of vascular risk factors.
Existing therapy options
Most symptoms of SVT go away on their own, no treatment is needed. Sometimes it is possible to stop the symptoms with the help of various measures, including drinking cold water, holding your breath or dipping your face in cold water. However, if SVT lasts for a long time with severe symptoms, you should immediately go to the hospital.
There are several ways to manage tachycardia:
- Short-term.
- Long-term.
- Pharmacological.
Below, each of them is considered separately.
Short-term disease management
The goal of this treatment is to stop acute attacks. This can be achieved through maneuvers that increase tone. For example, you can apply a cold irritant to the skin of the face. Also, in diseases such assupraventricular form of paroxysmal tachycardia, carotid sinus massage can be done.

If these actions do not help, it is recommended to take one of these medicines:
- "Adenosine". It removes symptoms very quickly by blocking electrical impulses in the heart, but the downside is that the duration of its action is short. In rare cases, it can aggravate bronchospasm, cause atypical chest discomfort.
- Verapamil, Diltiazem. The drugs are administered intravenously over 2-3 minutes. They carry the risk of potentiating hypotension and bradycardia.
Long-term disease management
how is paroxysmal supraventricular tachycardia treated? Treatment is individualized based on the frequency, severity of episodes, and the impact of symptoms on quality of life.
Drugs are prescribed for patients who:
- Recurrent symptomatic episodes of SVT affecting quality of life.
- Symptoms were identified by ECG.
- Rare episodes of SVT, but the patient's professional activities can lead to the development of the disease.
Radiofrequency catheter ablation is recommended for most of these patients. It has a low risk of complications and is curative in most cases. The procedure usually takes 1.5 hours and can be performed under local anesthesia with sedation or under general anesthesia. Patients usually stay overnight in the hospital for cardiac monitoring and observation.
Pharmacological disease management
The goal of pharmacotherapy is to reduce the frequency of SVT episodes. Only a small proportion of patients can get rid of the symptoms of a disease such as supraventricular tachycardia. Treatment includes the following recommended drugs:
- atrioventricular nodal blocking drugs;
- antiarrhythmic drugs of class I and III.

Beta-blockers and calcium channel blockers (class II and IV) are not suitable first-line treatment for Wolff-Parkinson-White syndrome. Randomized trials have not shown clinical superiority of any one agent. But beta-blockers and calcium channel blockers are superior to Digoxin therapy, as they provide the best blocking effect in AVNRT in a state of high sympathetic nervous system tone. They should not be used in patients with WPW syndrome as they may promote rapid conduction through accessory pathways in atrial fibrillation, which may lead to ventricular fibrillation.
Treatment of patients with Wolff-Parkinson-White syndrome
For patients with WPW syndrome, there is an alternative to the above medicines. For the treatment of such a disease, it is recommended:
- Flecainide.
- Sotalol (II and III classes of action).
They are more effective than beta-blockers and calcium channel blockers in preventing SVT, but are associated with a small riskdevelopment of ventricular tachycardia. This risk is low in patients without structural heart disease, but complications occur in 1-3% of patients treated with Sotalol, especially those using high doses.

Amiodarone has no role in the long-term prevention of SVT in both Wolff-Parkinson-White syndrome and other types due to the high frequency of serious toxic effects on the body with long-term use.
Prevention of episodes of SVT
You can take medication daily to prevent SVT episodes. Various drugs can affect the electrical impulses in the heart. If a remedy does not help or causes side effects, seek medical advice. He will advise which medicine is necessary for your particular case.
You must inform the relevant authorities and stop driving if there is a possibility of experiencing symptoms of illness while driving. Do not take drugs to prevent SVT, this can aggravate the situation and cause other heart problems. The best prevention is to stress the cardiovascular system daily through exercise.