- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
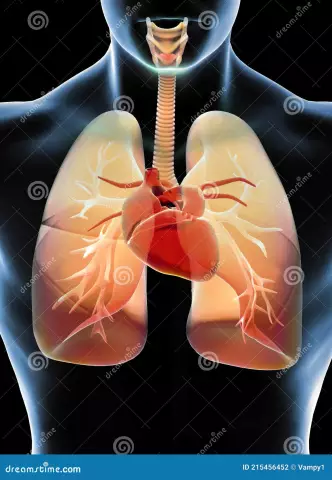
Fading heart - the treatment of this disease has recently worried the minds of many cardiac surgeons and other "heart" specialists. What is the reason for this, what are the symptoms of this dangerous disease, how to treat it - these are just some of the questions of interest to our citizens. It's no secret that a fairly large number of people have such a diagnosis as "heart failure". Symptoms, treatment with folk remedies, contacting specialized institutions, diagnoses - these concepts should be studied by everyone who has signs of the disease. Some of the current issues on this topic are highlighted below.
Fading heart: causes and treatment
The reason for the feeling of "fading" in the work of the heart can be various rhythm and conduction disturbances. Some of these conditions do not require medical attention, and for other forms, a delay in detection and treatment can be fatal. Distinguish between supraventricular and ventricular arrhythmias.

Supraventricular extrasystole
This is premature electrical activity of the heart. The reason isa source that is located in the atria, pulmonary and hollow veins, as well as in the atrioventricular junction. After such an extraordinary contraction, an incomplete or complete post-extrasystolic pause may develop. Frequent extrasystoles and a longer pause after an extraordinary contraction can give a feeling of fading, interruptions in the work of the heart.
These forms of arrhythmia have no independent clinical significance, except when their appearance is the start for triggering supraventricular tachycardia, flutter or atrial fibrillation.
In the absence of structural disorders in the heart muscle, special treatment of supraventricular extrasystoles is not required. In cases where they are accompanied by significant subjective discomfort, beta-blockers, verapamil, sedatives can be used.
Supraventricular extrasystoles are often a manifestation of the underlying disease (vegetovascular dystonia, chronic obstructive pulmonary disease, electrolyte disturbances), then the diagnosis and treatment of the underlying process is required.

Ventricular extrasystolic arrhythmia
Ventricular extrasystole - early electrical activity of the heart in relation to the main rhythm, stimulated by an impulse that arose in the legs or divergences of the bundle of His, Purkinje orions or the working myocardium. After this process, full compensatory pauses develop much more often, which, as in the case of atrial extrasystoles, are felt in the form of “fading”. Ventricular processes of any gradation without organic heart disease are not a risk factor for sudden death, therefore they are not treated. The exception is he althy patients with hereditary syndromes (congenital lengthening or shortening of QT, Brugada syndrome, etc.).
Fading of the heart, the causes and symptoms of which are discussed here, also occurs as a result of rare heart rhythms. Normal heart rate is determined in the range of 60 to 100 beats per minute. Physiological slowdown of the heart can develop during sleep, with deep breathing, in athletes.
If there is a violation at any stage of the generation and conduction of a heart impulse, pathological bradycardia develops, which can be symptomatic, asymptomatic and most often needs treatment.
Causes of bradycardia
Distinguish between internal and external causes of bradycardia. Internal causes include:
- aging;
- coronary heart disease;
- connective tissue diseases;
- congenital diseases, including atrioventricular node weakness;
- muscular amyloidosis;
- surgical trauma (bioprosthetic valve, heart transplant);
- contagious diseases (diphtheria, rheumatic heart disease, blood poisoning, typhoid fever).
External factors in the development of bradycardia include:
- physical fitness;
- exacerbated vagal electrotonus (vasovagal blackouts; hypersensitivity of the carotid sinus);
- drugs (beta blockers, calcium channel blockers, digoxin, lithium,antiarrhythmic substances);
- cocaine use;
- hypokalemia;
- hyperkalemia;
- neurological disorders (tumors of the central nervous system, increased intracranial pressure);
- obstructive sleep apnea syndrome.
For the diagnosis of bradycardias, Holter monitoring, incident counters and implantable recording devices, as well as an electrophysiological study are used.

Treatment of bradycardias
The first step is to identify the causes of bradycaridia and possibly eliminate them (discontinuation of beta-blockers). If there is no treatable cause, then medical therapy or temporary or permanent pacing may be needed.
Medicated treatment
Atropine, isoproterenol, aminophylline are used to stimulate the heart rate with significant slowdowns (longer than 3 seconds). However, these drugs can cause arrhythmias, including life-threatening ventricular failure. In patients with myocardial infarction and bradycardia due to ischemia, provide anti-ischemic therapy and take a wait-and-see approach, using pacing if necessary.
Patients with depressed sinus syndrome and atrioventricular block are being evaluated for temporary or permanent pacemakers. There is a developed European indication for permanent pacemakers in patients with SVS, AV block.

Varieties of stimulants
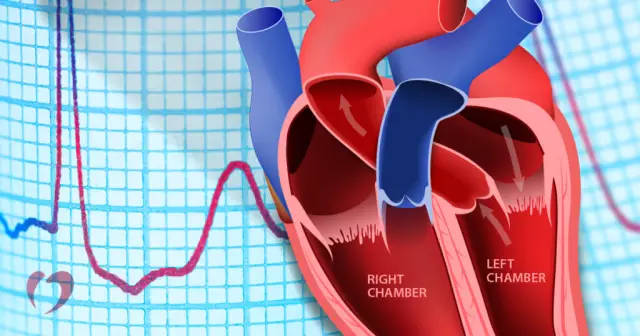
Distinguish single-chamber, two-chamber, three-chamber stimulators. The first and second have 1 and 2 electrodes (atrial and/or right ventricular). Three-chamber devices are used for biventricular activation and have an additional lead for the left ventricle.
When pacing the right atrium, the synchrony of ventricular contraction is disrupted. On the ECG during this process, the isolation of the right leg of the bundle of His is recorded. When both ventricles are stimulated, their synchronous work is preserved, cardiac hemodynamics in this case is much better.

Implantation
The first such device was installed in 1958. Subsequently, their evolution took place. Now these are modern, very small, high-tech devices.
Currently, between 400 and 1200 stimulants per million population are installed annually.
Cardiodevice conducts electrical activation of the myocardium. The signal propagates through the heart muscle in a non-physiological way. Its prolonged exposure can cause electrical and mechanical changes in the myocardium. Therefore, the installation of a stimulator must be carried out according to serious indications.

Features of stimulation modes
During right ventricular stimulation, an electrical impulse is applied to the apex of the left ventricle and depolarizes the slow-conducting myocardium. On the ECG, this is expressed by the blockade of the left leg of the bundleGisa. Such patients have a lower ejection fraction than patients without blockade. Also during this process, electrical remodeling of the heart occurs. Recently, there has been a trend towards a decrease in indications for the installation of these stimulants due to a significant number of adverse changes.
It has been established that the lowest ejection fraction is formed when exposed to the ventricles. Medium - when the atria are activated, then the rest of the heart. The highest ejection fraction is maintained during stimulation of the atria and ventricles along the natural pathways.
Fibrillation has been shown to be less in patients with atrial and dual chamber activation than in patients with only ventricular device exposure.
Dual chamber device proven by studies and experiments to be better in physically active patients. Pacemakers are currently the gold standard in the treatment of patients with symptomatic bradycardia. The search for the most physiological ways to positively influence the myocardium continues.

Conclusion
Thus, heart failure (during falling asleep or in other situations) is a very dangerous disease. At the first symptoms of this disease, you should immediately contact a medical institution, conduct all tests and be carefully treated. The sooner treatment and prevention begin, the more effective treatment procedures will be.