- Author Curtis Blomfield [email protected].
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
This disease is one of the stages in the development of acute pyelonephritis. With apostematous pyelonephritis, inflammatory processes occur, in which multiple purulent small abscesses (apostemes) are formed. The main place of their localization is the cortex of the kidneys.

Primary form
Most often, apostematous pyelonephritis begins to develop with obstruction of the ureter, less often with undisturbed urinary outflow.
In the kidney, small pustules are formed in the following way: microorganisms settle in the capillary loops of the glomeruli, in the terminal vessels of the kidney and in the peritubular capillaries. In this case, bacterial blood clots are formed, they then serve as a source of pustules. They are located on the surface of the renal cortex, as well as under the fibrous capsule in large quantities. On examination, they are clearly visible. Apostemes are yellowish in color, up to 2 mm in size, can be arranged in groups or singly.
With apostematous pyelonephritis, the kidney increases in size, has a cherry color. Perirenal tissue has edema, thickening of the fibrous capsule occurs. Pustules are visible on the section of the kidney, you can also find them in the medulla.

Apostematous pyelonephritis, carbuncle and kidney abscess
The second form of the disease is the carbuncle of the kidney. There is a purulent necrotic lesion of the organ, an abscess of the kidney. In the cortex, foci of necrosis are formed. Carbuncle can occur with a hematogenous route of infection. In such cases, the causes of apostematous pyelonephritis are pustular diseases, carbuncle, furunculosis, mastitis, panaritium. The mechanism of carbuncle formation is as follows:
- A bacterial thrombus enters the renal artery from a distant focus of pus, so a carbuncle appears in one of the blood supply areas of the arterial branch or in smaller arterial branches.
-
Carbuncle can develop when a large intrarenal vessel is compressed by an inflammatory infiltrate or due to contact with an inflammatory focus in the vessel wall.
The most common micro-organisms that cause carbuncle development are Staphylococcus aureus, Staphylococcus aureus, Proteus, and Escherichia coli.
On the section of the kidney, the carbuncle is visible as a rounded bulge from necrotic tissue, it is penetrated by merged small pustules, wedge-shaped extending deep into the parenchyma.
Acute apostematous pyelonephritis most often combines carbuncle of the kidney and apostematous pyelonephritis. There is no significant difference in clinical manifestationsobserved.

Clinical picture of apostematous pyelonephritis
Symptoms of apostematous pyelonephritis and carbuncle depend on how impaired the outflow of urine from the kidney.
Most often, the primary form of pyelonephritis occurs suddenly, usually after an intercurrent infection. Chills, high temperature (up to 40 degrees), pouring sweat appear. The hectic nature of the fever predominates (the rise in temperature is replaced by a fall). Terrific chills can last up to one hour, more often occurs at the peak of the temperature rise. After the chill, with a decrease in temperature, profuse sweating begins. These symptoms may be mild during the first three days.
Further on, pain in the lower back begins to intensify. On palpation, the kidneys are clearly painful, possibly enlarged. Changes in the urine occur on the fifth day, bacteriuria, proteinuria, leukocyturia appear.
The blood picture is characterized by leukocytosis, granularity in leukocytes, increased ESR, anemia.
With a progressive process, sepsis may develop, which has metastatic foci of purulent inflammation in the liver, lungs, and brain.

Kidney carbuncle clinic
If the outflow of urine is not disturbed in the kidney where the carbuncle develops, the clinical picture is similar to an acute infectious process. The temperature rises to 40 degrees, a stunning chill and heavy sweat are characteristic. Weakness increases, breathing quickens, nausea and vomiting, tachycardia set in.
In the firstdays often there is no pain in the lower back, bacteriuria, leukocyturia, dysuric disorders are not observed. Diagnosis is difficult. Patients can get treatment in therapeutic, infectious, surgical departments. A doctor may mistakenly diagnose pneumonia, acute cholecystitis, typhoid fever, and the like. Only a few days later, when local symptoms begin to appear (lower back pain, Pasternatsky's symptom, pain on palpation), the doctor focuses on the kidneys.

Apostematous pyelonephritis, diagnosis
Diagnosis of the disease is based on the following indicators:
- febrile period lasts more than three days;
- enlarged painful kidney on palpation;
- laboratory tests: bacteriuria, leukocyturia, in the blood - a shift to the left of the leukocyte formula, leukocytosis, C-reactive protein, an increase in ESR;
- excretory urogram - decrease in kidney function, increase on the affected side;
- Ultrasound - restriction of mobility, increase in the size of organs, thickening of the parenchyma by more than 2 cm, its heterogeneous density; fluid in the perinephric space, the pelvicalyceal system expands with obstruction of the ureter;
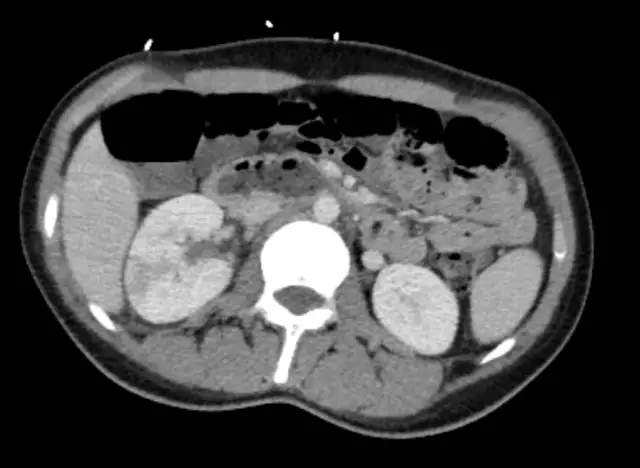
- MSCT, MRI, CT - increase in the size of the kidney, thickening of the parenchyma, its heterogeneity, manifestation of foci of purulent destruction;
- dynamic and static nephroscintigraphy - an increase in the size of the kidneys, uneven accumulation of the isotope in the parenchyma.
Purulent tissue destructionmore clearly detected with carbuncle. On ultrasound in the parenchyma, foci of increased density are clearly visible, as well as their mixed structure. This picture is clearly visible on MRI, CT. Contrast-enhanced helical CT makes it possible to see abnormalities when contrast enters necrosis foci.
Evaluation difficulties
Difficulties in assessing the patient's condition may arise if, prior to admission to urology, the patient underwent antibacterial therapy with modern antibiotics for one to two weeks. Such treatment can smooth out the manifestations of apostematous pyelonephritis, but there will be no cardinal improvement in the condition. The body temperature drops, the pain syndrome decreases, chills rarely occur, their character is less pronounced and prolonged. The number of leukocytes in the blood decreases, but the shift to the left of the leukocyte formula is still preserved, as is anemia and increased ESR. In other words, the disease manifests itself as a sluggish sepsis. This "improvement" is the cause of mismanagement. To prevent the development of severe sepsis, if there is a focus of destruction in the kidney, the patient must be operated on.

Differential Diagnosis
When apostematous pyelonephritis is detected, it is necessary to differentiate this disease from other infectious ones. With acute pancreatitis and cholecystitis, subphrenic abscess, acute appendicitis, acute cholangitis, acute adnexitis and acute pleurisy.
Kidney curbuncle differentiates from a simple festering kidney cyst, with a tumorparenchyma, with acute diseases of the abdominal cavity.
What distinguishes apestomatous pyelonephritis and renal carbuncle?
- Leukocyturia. Bacteriuria.
- Lower pain.
- Impaired kidney function.
- Thickening of the parenchyma. Changes in its density.
- Painful palpation with kidney enlargement.
- Expansion of the pelvicalyceal system.
US, MRI, CT data allow us to distinguish apostematous pyelonephritis from various acute diseases of the peritoneum.
Treatment
Treatment of apostematous pyelonephritis and carbuncle is carried out exclusively by surgery. Most often, the operation is performed on an emergency basis. Preliminary short-term preoperative preparation with the participation of an anesthesiologist-resuscitator lasts no more than two hours. Preparation includes:
- Catheterization of the pelvis, intravenous administration of an antibiotic.
- Transfusion of glucose and electrolytes.
- Stabilization of blood pressure.
- According to indications - cardiotonic.
The main goal of the operation is to prevent sepsis. Saving a life.
Secondary goal is to save the kidney.
An endotracheal anesthesia is used for pain relief.
During the operation, the contents of abscesses and the pelvis are taken to make a culture for the determination of microflora to further determine sensitivity to antibiotics. The results will confirm purulent pyelonephritis, as well as determine further treatment tactics.

Postoperativeperiod
After the operation, the patient receives treatment taking into account the inhibition of kidney function and intoxication. The patient is assigned:
- 10% glucose solution - 500 ml, with 10 units of insulin IV;
- solution 9% sodium chloride - 1000 ml;
- Hemodez - 400 ml;
- cocarboxylase - up to 200 mg;
- vitamin B6 - up to 2 ml;
- vitamin C - up to 500 mg;
- Korglicon solution 0.06% to 1.0 ml;
- mannitol solution 15% to 50 ml;
- Lasix up to 60 mg;
- fresh frozen (native) plasma - 250 ml;
- Clexane or Fragmin, taking into account coagulation parameters;
- erythrocyte mass for anemia (Hb less than 70).
For purulent intoxication, extracorporeal detoxification is used (plasmapheresis, hemosorption, plasmasorption).
Antibacterial therapy with two broad spectrum antibiotics is required.
When assessing the state of the parenchyma, the most modern methods are used (MRI, CT, ultrasound). This makes it possible to correctly assess the situation and choose the most adequate volumes of the operation.