- Author Curtis Blomfield [email protected].
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
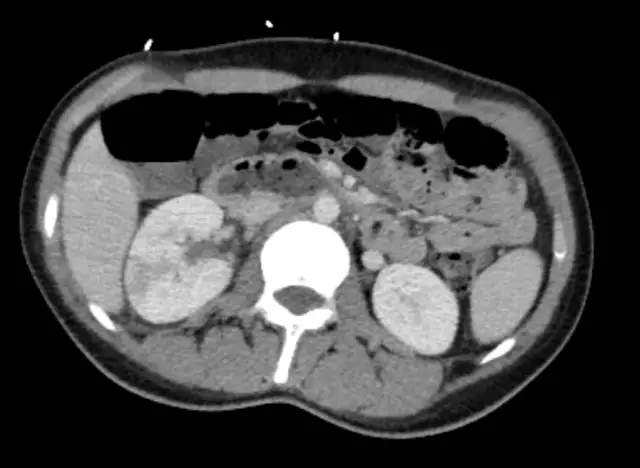
One of the most common kidney diseases is pyelonephritis. Pathology is a vast process. Inflammation covers the pelvis and calyces of the kidneys, as well as connective (interstitial) tissue. Infection occurs either from the outside, through the urinary system, or by the hematogenous route (with blood flow) from other foci. Next, we will analyze how pyelonephritis manifests itself. Treatment, drugs to eliminate it will also be described in the article.

General information
The main causative agents of pyelonephritis are bacteria of the staphylococcus group, Escherichia and Pseudomonas aeruginosa, Proteus, Streptococcus, Enterococcus. The development of pathology under the influence of fungi or viruses is much less common. Often pyelonephritis is provoked by microbial associations or pathogens of L-forms. The latter are characterized by a non-enveloped adaptive state, characterized by high resistance to drugs. This significantly complicates not only therapy, but also diagnosis.pathology. The disease quickly passes from the acute to the chronic stage. In this regard, antibiotics for pyelonephritis of the kidneys should be prescribed as early as possible.
Therapeutic interventions
Any antibiotic for pyelonephritis should have a wide range of therapeutic activity, high bactericidal action, minimal nephrotoxicity. The drug should also be excreted in the urine in large volumes. The list of antibiotics prescribed for the described pathology includes aminopenicillins, protected penicillins, cephalosporins, carboxypenicillins, aminoglycosides, fluoroquinolones. Next, consider which antibiotics for pyelonephritis are most often prescribed.

Aminopenicillins
Specialists today try not to prescribe these drugs for pyelonephritis. They are characterized by increased natural activity against Proteus, Escherichia coli, enterococci. Their main disadvantage is considered to be susceptibility to the influence of beta-lactamases - enzymes produced by many clinically significant pathogens. Today, these antibiotics are not recommended for inflammation of the kidneys (except for pathology in pregnant women) due to the increased level of resistant (resistant) strains of Escherichia coli (more than 30%) to them.
Protected penicillins
These antibiotics for inflammation of the kidneys are considered the means of choice. Medicines show high activity both relative to gram-negative microorganisms that produce beta-lactamase, and gram-positive bacteria, including staphylococcipenicillin-resistant and coagulase-negative. The level of resistance exhibited by E. coli strains to protected penicillins is relatively low. An antibiotic is often prescribed for pyelonephritis "Amoxicillin" and the remedy "Clavulanate". This combination is recommended orally at 625 mg / 3 rubles / day. or parenterally at 1.2 g / 3 rubles / day. Duration of therapy - from seven to ten days. An innovative form of this combination is considered to be an antibiotic for pyelonephritis "Flemoklav Solutab". The drug has proven effectiveness in urinary tract infections. Means "Flemoklav Solutab" is allowed for use by patients from three months and pregnant women.

Medicines for complicated forms
In severe cases and if an infection caused by Pseudomonas aeruginosa is suspected, carboxypenicillins may be prescribed. In particular, it is such an antibiotic for pyelonephritis as "Ticarcillin". In the same group is the drug "Carbenicillin". In addition to carboxypenicillins, ureidopenicillins may be recommended. These include such medicines as Azlocillin, Piperacillin. However, it should be noted that antipseudomonal penicillins are not recommended as mono-drugs. This is due to the high probability of developing resistance of microorganisms to them in the course of therapy. In the treatment of pyelonephritis, combinations of these drugs and beta-lactamase inhibitors are used. In particular, combinations of the following agents are prescribed:"Ticarcillin" + clavulanic acid, "Tazobactam" + "Piperacillin". Combinations of antipseudomonal antibiotics with fluoroquinolones and aminoglycosides are also used. Such medications are also prescribed for severe hospital infectious pathologies of the urinary system.

Cephalosporins
These drugs have the ability to accumulate in the kidney parenchyma and urine in fairly high concentrations. Cephalosporins are moderately nephrotoxic. These drugs are in the lead today in terms of the frequency of prescription in patients with pyelonephritis and infections of the urinary system. There are several generations of cephalosporins. They are divided according to the spectrum of action and the degree of resistance to beta-lactamase:
- 1st generation. These drugs have a relatively limited spectrum of activity. They act mainly on gram-positive cocci and are not used in the acute course of the pathology.
- 2nd generation. These cephalosporins have a wider spectrum of action. They are active against Escherichia coli and a number of other enterobacteria. The drugs of this group include, for example, the drug "Cefuroxime".
- 3rd generation. Cephalosporins of this group are used for complicated infections. Medications are prescribed both orally (Ceftibuten, Cefixime) and parenterally (Ceftriaxone,"cefotaxime"). In the latter case, a longer half-life is characteristic and the use of two routes for excretion from the body: with urine and bile. In the group of third-generation cephalosporins, there are drugs that are active against Pseudomonas aeruginosa. These are, in particular, such drugs as Cefoperazone, Ceftazidime, as well as the inhibitor-protected drug Cefoperazone + Sulbactam.
- 4th generation. Cephalosporins of this group have all the properties of the drugs of the previous category, but at the same time they are more active in relation to gram-positive cocci.

Aminoglycosides
These medicines are recommended for complicated forms of pyelonephritis, as well as serious nosocomial infections. The group of aminoglycosides includes such agents as Amikacin, Tobramycin, Netilmicin, Gentamicin. In severe cases, these medicines are combined with cephalosporins and penicillins. Aminoglycosides are poorly absorbed from the gastrointestinal tract. In this regard, they are administered mainly parenterally. Excretion of drugs is carried out unchanged in the urine. For patients with renal insufficiency it is necessary to adjust the dosage. The disadvantages of aminoglycosides include their pronounced nephro- and ototoxicity. The frequency of hearing impairment in patients reaches 8%, and kidney damage (manifested as neoliguric, usually reversible insufficiency) - 17%. This makes it necessary to ensure control over the level of urea during therapy,potassium, creatinine. Due to the fact that the dependence of the severity of complications on the concentration of drugs in the blood has been established, a single administration of the full daily dosage is used. Such a scheme, among other things, helps to reduce the likelihood of developing a nephrotoxic effect. The factors that cause this complication include:
- Repeating medication less than a year apart.
- Old age.
- Long-term diuretic treatment.
- Complex use with drugs from the group of cephalosporins in high dosages.

Fluoroquinolones
These medications have been the drugs of choice in recent years. They are prescribed both in outpatient and inpatient settings. The first generation fluoroquinolones include drugs such as Ciprofloxacin, Pefloxacin, Ofloxacin. They are active against most infectious agents in the genitourinary system. The advantage of drugs is their low toxicity, long half-life, which, in turn, allows you to take them twice a day. Fluoroquinolones are satisfactorily tolerated by patients; they form sufficiently high concentrations in urine, kidney tissue, and blood. Medicines are used both parenterally and orally, except for Norfloxacin (it is intended for oral administration). Fluoroquinolones of the second generation (drugs "Lomefloxacin", "Levofloxacin", "Moxifloxacin" and others)are distinguished by greater activity relative to gram-positive microorganisms, pneumococci primarily. At the same time, they have the same strong effect on gram-negative bacteria (except for Pseudomonas aeruginosa) as well as drugs of the previous generation.

Prevention of pyelonephritis
In order to avoid recurrence or the primary occurrence of pathology, it is necessary to eliminate all alleged provoking factors. Prevention of pyelonephritis includes a whole range of measures. This includes the normalization of diet, rest and work, sleep and wakefulness. A prerequisite is the absolute exclusion of hypothermia. Particular attention should be paid to the general condition of the body - it is important that there are no infections in it. In this regard, treatment of probable diseases should be carried out: colitis, caries, gastritis and others.