- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
Different people have different ability of insulin to stimulate the uptake of glucose. It is important to know that a person may have normal sensitivity to one or more of the effects of this compound and at the same time be completely resistant to others. Next, we will analyze the concept of "insulin resistance": what it is, how it manifests itself.

General information
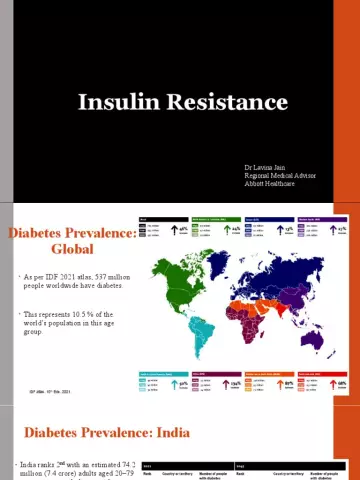
Before analyzing the concept of "insulin resistance", what it is and what signs it has, it should be said that this disorder occurs quite often. More than 50% of people with hypertension suffer from this pathology. Most often, insulin resistance (what it is, will be described below) is found in the elderly. But in some cases it comes to light and in the childhood. The syndrome of insulin resistance often remains unrecognized until metabolic disorders begin to appear. The risk group includes people with dyslipidemia or impaired glucose tolerance, obesity, hypertension.
Insulin resistance
What is this? What are the features of the violation? The metabolic syndrome of insulin resistance is an incorrect response of the body to the action of one of the compounds. The concept is applicable to different biological effects. This, in particular, refers to the effect of insulin on protein and lipid metabolism, gene expression, and the function of the vascular endothelium. The disturbed response leads to an increase in the concentration of the compound in the blood relative to that required for the available amount of glucose. Insulin resistance syndrome is a combined disorder. It involves changes in glucose tolerance, type 2 diabetes, dyslipidemia, and obesity. "Syndrome X" also implies resistance to glucose uptake (insulin-dependent).

Development mechanism
To date, specialists have not been able to fully study it. Disorders that lead to the development of insulin resistance can occur at the following levels:
- Receptor. In this case, the condition is manifested by affinity or a decrease in the number of receptors.
- At the level of glucose transport. In this case, a decrease in the number of GLUT4 molecules is revealed.
- Prereceptor. In this case, they speak of abnormal insulin.
- Post-receptor. In this case, there is a violation of phosphorylation and a violation of signal transmission.
Abnormal insulin molecules are quite rare and have no clinical significance. Receptor density may be reduced in patients due tonegative feedback. It is caused by hyperinsulinemia. Often, patients have a moderate decrease in the number of receptors. In this case, the level of feedback is not considered a criterion by which the degree of insulin resistance is determined. The causes of the disorder are reduced by experts to post-receptor signal transduction disorders. Provoking factors, in particular, include:
- Smoking.
- Increase in TNF-alpha.
- Reduce physical activity.
- Increased concentration of non-esterified fatty acids.
- Age.

These are the main factors that more often than others can provoke insulin resistance. Treatment includes:
- Diuretics of the thiazide group.
- Beta-adrenergic blockers.
- Nicotinic acid.
- Corticosteroids.
Increased insulin resistance
Influence on glucose metabolism occurs in adipose tissue, muscle and liver. Skeletal muscle metabolizes approximately 80% of this compound. Muscles in this case act as an important source of insulin resistance. Glucose is taken up into cells by a special transport protein, GLUT4. Activation of the insulin receptor triggers a series of phosphorylation reactions. They ultimately lead to the translocation of GLUT4 into the cell membrane from the cytosol. This allows glucose to enter the cell. Insulin resistance (the norm will be indicated below)due to a decrease in the degree of GLUT4 translocation. At the same time, there is a decrease in the use and uptake of glucose by cells. Along with this, in addition to facilitating glucose uptake in peripheral tissues, hyperinsulinemia suppresses the production of glucose by the liver. With type 2 diabetes, it resumes.
Obesity
It is combined with insulin resistance quite often. When the patient exceeds the weight by 35-40%, the sensitivity decreases by 40%. The adipose tissue located in the anterior abdominal wall has a higher metabolic activity than the one located below. In the course of medical observations, it has been established that increased release of fatty acids from the abdominal fibers into the portal bloodstream provokes the production of triglycerides by the liver.

Clinical signs
Insulin resistance, the symptoms of which are predominantly metabolically related, may be suspected in patients with abdominal obesity, gestational diabetes, family history of type 2 diabetes, dyslipidemia, and hypertension. At risk and women with PCOS (polycystic ovaries). Due to the fact that obesity is a marker of insulin resistance, it is necessary to assess the nature of the distribution of fatty tissue. Its location can be gynecoid - in the lower part of the body, or android type - in the anterior wall of the peritoneum. Accumulation in the upper half of the body is a more significant predictor of insulin resistance, altered glucose tolerance, and DM than obesity inlower areas. To determine the amount of abdominal fat, you can use the following method: determine the ratio of waist, hips and BMI. With indicators of 0.8 for women and 0.1 for men and a BMI greater than 27, abdominal obesity and insulin resistance are diagnosed. Symptoms of pathology are also manifested externally. In particular, wrinkled, rough hyperpigmented areas are noted on the skin. Most often they appear in the armpits, on the elbows, under the mammary glands. The analysis for insulin resistance is a calculation according to the formula. HOMA-IR is calculated as follows: fasting insulin (μU/mL) x fasting glucose (mmol/L). The result obtained is divided by 22.5. The result is an index of insulin resistance. The norm is <2, 77. If there is an upward deviation, a tissue sensitivity disorder can be diagnosed.

Disorders of other systems: vascular atherosclerosis
Today there is no single explanation of the mechanism of the influence of insulin resistance on the damage to the cardiovascular system. There may be a direct effect on atherogenesis. It is caused by the ability of insulin to stimulate lipid synthesis and the proliferation of smooth muscle components in the vascular wall. At the same time, atherosclerosis can be caused by concomitant metabolic disorders. For example, it can be hypertension, dyslipidemia, changes in glucose tolerance. In the pathogenesis of the disease, the impaired function of the vascular endothelium is of particular importance. Its mission is to maintaintone of the blood channels due to the secretion of mediators of vasodilation and vasoconstriction. In a normal state, insulin provokes relaxation of the smooth muscle fibers of the vascular wall with the release of nitric oxide (2). At the same time, its ability to enhance endothelium-dependent vasodilation changes significantly in obese patients. The same applies to patients with insulin resistance. With the development of the inability of the coronary arteries to respond to normal stimuli and expand, we can speak of the first stage of microcirculation disorders - microangiopathy. This pathological condition is observed in most patients with diabetes (diabetes mellitus).

Insulin resistance can provoke atherosclerosis through disturbances in the process of fibrinolysis. PAI-1 (plasminogen activator inhibitor) is found in high concentrations in diabetic and obese patients without diabetes. The synthesis of PAI-1 is stimulated by proinsulin and insulin. Fibrinogen and other procoagulant factors are also increased.
Altered glucose tolerance and type 2 diabetes
Insulin resistance is a precursor to the clinical manifestation of DM. Beta cells in the pancreas are responsible for lowering glucose levels. The decrease in concentration is carried out by increasing the production of insulin, which, in turn, leads to relative hyperinsulinemia. Euglycemia can persist in patients for as long as the beta cells are able to maintain a sufficiently high plasma insulin level toovercome resistance. Ultimately, this ability is lost, and the concentration of glucose increases significantly. The key factor responsible for fasting hyperglycemia in T2DM is hepatic insulin resistance. The he althy response is to lower glucose production. With insulin resistance, this reaction is lost. As a result, the liver continues to overproduce glucose, leading to fasting hyperglycemia. With the loss of the ability of beta cells to provide hypersecretion of insulin, there is a transition from insulin resistance with hyperinsulinemia to altered glucose tolerance. Subsequently, the condition is transformed into clinical diabetes and hyperglycemia.
Hypertension
There are several mechanisms that cause its development against the background of insulin resistance. As observations show, the weakening of vasodilation and the activation of vasoconstriction can contribute to an increase in vascular resistance. Insulin stimulates the nervous (sympathetic) system. This leads to an increase in the plasma concentration of norepinephrine. Patients with insulin resistance have an increased response to angiotensin. In addition, the mechanisms of vasodilation may be disturbed. In a normal state, the introduction of insulin provokes relaxation of the muscular vascular wall. Vasodilation in this case is mediated by the release/production of nitric oxide from the endothelium. In patients with insulin resistance, endothelial function is impaired. This leads to a decrease in vasodilation by 40-50%.

Dyslipidemia
With insulin resistance, the normal suppression of the release of free fatty acids after eating from adipose tissue is disrupted. The increased concentration forms a substrate for enhanced triglyceride synthesis. This is an important step in the production of VLDL. With hyperinsulinemia, the activity of an important enzyme, lipoprotein lipase, decreases. Among the qualitative changes in the spectrum of LDL against the background of type 2 diabetes and insulin resistance, an increased degree of oxidation of LDL particles should be noted. Glycated apolipoproteins are considered to be more susceptible to this process.
Therapeutic interventions
Increased insulin sensitivity can be achieved in several ways. Of particular importance is weight loss and physical activity. Diet is also important for people diagnosed with insulin resistance. The diet helps to stabilize the condition within a few days. Increased sensitivity will further contribute to weight loss. For people who have established insulin resistance, treatment consists of several stages. Stabilization of diet and physical activity is considered the first stage of therapy. For people who have insulin resistance, the diet should be low in calories. A moderate decrease in body weight (by 5-10 kilograms) often improves glucose control. Calories are 80-90% distributed between carbohydrates and fats, 10-20% are proteins.
Drugs
Means "Metamorphin" refers to medicines of the biguanide group. The drug helps to increaseperipheral and hepatic sensitivity to insulin. In this case, the agent does not affect its secretion. In the absence of insulin, Metamorphin is ineffective. Troglitazone is the first thiazolidinedione drug to be approved for use in the United States. The drug enhances the transport of glucose. This is probably due to the activation of the PPAR-gamma receptor. And due to this, the expression of GLUT4 is enhanced, which, in turn, leads to an increase in insulin-induced glucose uptake. For patients who have insulin resistance, treatment can be prescribed and combined. The above agents may be used in combination with a sulfonylurea, and sometimes with each other, to obtain a synergistic effect on plasma glucose and other disorders. The drug "Metamorphine" in combination with a sulfonylurea enhances the secretion and sensitivity to insulin. At the same time, glucose levels decrease after meals and on an empty stomach. Patients treated with combination therapy were more likely to experience hypoglycemia.