- Author Curtis Blomfield [email protected].
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
Septic pneumonia is a very severe form of pneumonia that develops as a result of sepsis. The main predisposing factor to the appearance of a dangerous pathology is the presence of serious disorders in the patient's immune system. The risk group includes the elderly, newborns with intrauterine infection and HIV-infected. It is worth noting that infectious pneumonia often ends in death. The article describes this disease. Readers will also learn about the symptoms and treatment of septic pneumonia.
What is this

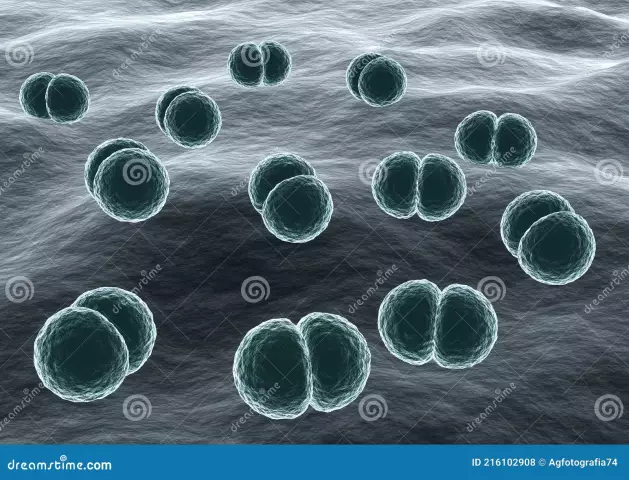
Sepsis is understood as an inflammatory reaction of the body in response to any infection. This condition occurs when toxins or pathogens enter the bloodstream. In this case, the infection spreads and damage to various systems andorgans, including the lungs, which provokes infectious pneumonia.
In addition to pathogens, causes of sepsis can be:
- pathogenic fungi;
- various bacteria (Streptococcus, Staphylococcus, Proteus, Pneumococcus, Enterococcus, Klebsiella and others);
- viruses.
Patients with infectious pneumonia are rushed to the intensive care unit upon admission to the hospital.
Reasons
The following factors contribute to the development of septic pneumonia:
- Hypothermia. It is worth noting that this reason is relevant not only in the cold season. It often poses a danger in the warm period. Examples are: body hypothermia due to cold water, room air conditioning, and so on.
- SARS is one of the most common causes of septic pneumonia as a complication of a viral disease. This may occur due to incomplete or inadequate treatment, as well as the addition of other pathogens.
- Active and passive smoking. This bad habit leads to a weakening of the lung tissue, as well as immunity in general.
- Negative manifestation of the external environment, including air pollution with toxic substances.
In addition to these factors, each person has a threshold of individual resistance, and there are also chronic or concomitant diseases that aggravate the condition of the body. These causes can contribute to the development of pneumonia, and the course of the disease itself becomes more severe. In childhood and old age, septic pneumonia often causes complications.
Individual factors

This group of causes contributing to the emergence of infectious pneumonia include:
- Chronic lung disease.
- Pathologies of the heart and blood vessels associated with circulatory disorders in the pulmonary circle.
- Congenital anomalies of the chest, as well as its injuries.
- Recovery period after surgery.
- Bad habits (alcohol, drugs, smoking).
- Reduced immunity.
- Age.
Symptoms of disease
In most people, septic pneumonia (ICD-10 - code - from J12 to J18) is accompanied by purulent decay of the lung tissue. Sepsis significantly worsens the already serious condition of the patient.

Main clinical signs that may indicate infectious inflammation are:
- fever, fever, chills;
- violent cough, often causing chest pain;
- shortness of breath;
- shortness of breath;
- respiratory failure that progresses with improper treatment;
- skin turns pale and cyanotic;
- rapid heart rate;
- a sharp drop in pressure;
- breakthrough of an abscess in the bronchi can cause a strong cough, while the patient will cough up a lot of purulent sputum.
To complicationsseptic pneumonia include pyopneumothorax, pulmonary hemorrhage, pleural empyema, bacteremic shock. All this, with untimely treatment, can lead to death.
Bilateral septic pneumonia
In medical practice, bilateral pneumonia are classified according to several criteria. The main criterion is the location of the foci of inflammation. Based on this, there are several types of such pneumonia:
- focal;
- total.
The latter is less common than focal, and is characterized by the rapid development of the inflammatory process, as well as a pronounced clinical picture. This form of the disease involves the defeat of both lungs in full, so respiratory failure and death of the patient occur quickly enough.

Focal bilateral septic pneumonia is much more common. When it occurs, the defeat of some segments of the lung on both sides. This form of inflammation can be the result of mechanical ventilation for an extended period, so it is common among people in intensive care. Unfortunately, the prognosis for recovery with focal pneumonia in the lungs on both sides is extremely unfavorable. Since numerous areas are affected in the respiratory organ.
If we classify inflammation of the lungs, taking into account which area is affected, we can distinguish the following forms of the disease:
- upper lobar bilateral;
- lower lobe bilateral;
- polysegmental.
The most dangerous course is a polysegmental type of inflammation in both lungs. The disease is severe, with signs of severe intoxication, and therefore therapy should begin as early as possible. It should be borne in mind that polysegmental inflammation quickly leads to respiratory failure and death of the patient.
The most formidable complication of bilateral septic pneumonia is HIT (immediate type hypersensitivity). It often leads to pulmonary edema with respiratory failure.
Diagnosis of disease

The main method for diagnosing inflammation of the lungs is x-ray. Signs of septic pneumonia in this case look like multiple foci of blackout. As a rule, they are interconnected and form abscesses. X-ray studies are used not only for diagnostic purposes, but also to assess the dynamics of the disease.
During the initial examination, the doctor can determine the involvement of accessory muscles in breathing and an increase in the frequency of the respiratory process. In addition, the specialist distinguishes between wheezing: dry, wet or crepitant. X-ray does not always help to see the foci of inflammation. After all, they can have a deep location and small sizes. That is why in some cases additional diagnostic methods are needed. For this, angiography, scintigraphy and computed tomography are used. CT is the best way to see septic pneumonia.
Besides the above methods,used to diagnose a disease:
- biochemical and clinical blood tests;
- general urinalysis;
- sputum test to determine bacterial resistance to antibiotics.
In case of urgent need, additional research is carried out:
- serological survey;
- histo- and cytological studies;
- bronchoscopy;
- angiopulmonography and isotope scanning of the lungs;
- if surgery is necessary, a test is taken for the proper functioning of the kidneys and liver to establish the range of loads on the heart and blood vessels.
Treatment of disease

Patients even with suspected infectious pneumonia are being treated and further examination in the intensive care unit. The general approach to the treatment of the disease and the very cause that provoked it, is to use all available surgical and therapeutic methods.
Intensive care begins the moment the patient enters the department. After determining the entrance gate of the infection, which led to the spread of the inflammatory process, the septic focus is eliminated. The main task of intensive care is to eliminate septic shock in pneumonia, as well as complications that threaten the stabilization of the patient's condition and life.
During the treatment process, doctors from different fields of medicine take part: therapists, resuscitators, surgeons and others.
Antibacterial therapy
The use of antibacterial drugs for infectious inflammation of the lungs significantly reduces the risk of complications and deaths. As a rule, doctors do not wait for the results of bacteriological tests, they prescribe broad-spectrum antibiotics immediately after the patient enters the department.
After identifying the causative agent of infection, antibiotic therapy is adjusted. This takes into account the sensitivity of pathogenic microflora to drugs. Most often, preference is given to medicines that have a bactericidal effect:
- Cephalosporinam.
- Penicillins.
- Fluoroquinolones.
- Carbapenem.
- Aminoglycosides and others.
In some cases, combined therapy with antibacterial drugs is used. But still, experts prefer monotherapy. Since the simultaneous use of several antibiotics increases the risk of side effects and compatibility problems. When choosing the optimal medicine, it is necessary to take into account contraindications, the presence of individual intolerance, toxic effects on the kidneys and liver, and so on.
Prescribing the maximum allowable dosage of antibiotics for septic pneumonia is considered clinically justified. To date, an empirical antibiotic therapy regimen has been developed that can be used even without the availability of research results.
In the absence of data on the pathogens of the infectious process, it is considered normal to use a combinationdifferent drugs. It is worth remembering that only a specialist can determine the correct combination of medicines.
Detoxification measures

An obligatory element of the treatment of septic pneumonia (ICD-10 - code - from J12 to J18) is effective detoxification therapy. The introduction of intravenous electrolyte solutions helps to correct the water-s alt balance. Protein disturbances in the body effectively restore albumin, amino acid preparations, and plasma. To eliminate toxins and pathogens, hemosorption, plasmapheresis and hemofiltration are used. In case of kidney failure, hemodialysis is prescribed.
Surgery
Some cases of septic pneumonia require surgical treatment. This is especially true in the event of severe complications. The indications for surgery are:
- Pneumothorax (accumulation of air in the pleural cavity).
- Development of bleeding in the lungs.
- Pus in the pleural cavity.
- Preservation of signs of septic pneumonia (hemoptysis, cough with purulent sputum, etc.) after the elimination of the infection for several months.
Competent treatment of septic pneumonia using modern methods of therapy allows you to count on a positive outcome even in the most severe cases.
Human Immunodeficiency Virus

Septic pneumonia develops with HIVin 80% of patients. This high percentage is due to the following factors:
- The main function of the lungs is breathing. Together with the air, viruses, bacteria, the smallest particles of dust get into them, so the concentration of pathogens of various diseases in the lungs is much higher than in other organs.
- Besides this, the lungs themselves do not have local immunity. Only the general immunity of the body is responsible for their protection, and with the human immunodeficiency virus it is weakened and cannot resist infections.
- The lungs have their own microflora, which is not dangerous for a he althy person. But due to a weakened immune system, these harmless fungi and bacteria can trigger the development of pneumonia.
The main goal of treating pneumonia in HIV patients is to restore immunity. In addition, antiretroviral therapy is being carried out.
Prevention of septic pneumonia in HIV should be lifelong. With a decrease in the level of CD4-lymphocytes, patients are prescribed Biseptol (once every three days). If the patient has already suffered infectious pneumonia, then Biseptol is taken daily.
In addition to drug prevention, it is recommended to follow a special regimen, diet, give up bad habits and regularly visit your doctor.
Forecast
Septic pneumonia is characterized by a long course and a tendency to reappear. Unfortunately, the prognosis for this disease is often poor. In half of the cases it ends in death. Attimely access to a doctor and proper treatment increases the chance of recovery.