- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
Modern diagnostics is not complete without ultrasound. You can confirm or refute the diagnosis using this procedure. This method allows you to look inside the human body and see what was previously impossible.
Base for holding

Most women go to the gynecologist due to he alth complaints. After the diagnosis in the office during the reception, in addition to tests, an ultrasound of the uterus or, as they say, the pelvic organs, is prescribed. This study is carried out in order to determine or establish the cause:
- failure in the menstrual cycle;
- pain in the abdomen, lower back, specific discharge and unpleasant odor from the genitals;
- bleeding mid cycle or after intercourse;
- inflammatory processes in the pelvic organs;
- infertility, problems with conception.
For example, an ultrasound of the uterus shows what needs to be done to stimulate the body to become pregnant. You can also track the degree of maturity of the follicles, on which dependsthe onset of ovulation, the readiness of the endometrium to accept a fertilized egg, the patency of the fallopian tubes.
Preparing for the study

Today, ultrasound of the uterus and appendages is done, as a rule, without preparation. This was made possible thanks to a modern intravaginal sensor. Therefore, filling the bladder is no longer required. If the study takes place in a city clinic, then most likely you will need to take with you a condom for ultrasound (it is called that, it is sold at a pharmacy), a diaper and socks. A condom is required for hygienic use of the transducer because it looks like a rod 12 cm long and 2-3 cm in diameter.
In a private clinic or medical center, usually all this is already included in the cost of the procedure. Therefore, a woman does not need to purchase anything in advance. In order to undergo a diagnosis, you just need to come to the reception.
Woman during the study is in a supine position, legs bent at the knees. Some discomfort may be felt as the transducer is brought close to the cervix and may touch it. The duration of the manipulations depends on whether the woman has any deviations and complaints.
In rare cases, when the above method cannot be applied to a particular patient, it is possible to conduct a study with a transabdominal probe (through the abdomen). This method just requires preparation in order for a clear picture to be displayed on the screen. A woman is asked to fill her bladderfor example, drink 0.5-1 liter of pure water or tea half an hour to an hour before the start of the study. Diagnostics is also carried out in the prone position, you do not need to bend your legs, just keep calm and not move. Unpleasant sensations may occur when pressing the sensor on the bladder.
There is also a transrectal sensor that can be used during the diagnosis of the condition of the pelvic organs. This method is resorted to if the patient is a virgin, and the study with a transabdominal sensor is not effective. The preparation process consists in the exclusion of products that form gases. Before the procedure, it is necessary to clean the intestines (for example, make a cleansing microclyster). The position to be taken during the diagnosis is on the side with legs bent at the knees. Discomfort may be felt during the insertion of the probe into the anus. Lubricant is used by the diagnostician to minimize pain.
Which day is best to go for research
In order for the ultrasound of the uterus to be informative, the gynecologist usually advises on which days it is necessary to undergo a diagnosis. As a rule, to determine any changes, small formations (cysts, polyps), abnormalities in the pelvic organs, it is recommended to conduct an examination in the first half of the cycle, after the end of menstrual bleeding.
If the reason for the ultrasound examination is a suspicion of endometriosis, then the optimal time for the procedure is the second half of the menstrual cycle. If there is suspicion ofa tumor or myoma ultrasound of the uterus is performed twice - at the beginning and at the end of the cycle. An emergency test is scheduled at any time.
What the results say
After the diagnosis, the specialist gives a conclusion. Deciphering the ultrasound of the uterus (and, if necessary, its appendages) is carried out by the attending physician. According to the specified data, he can determine if there are deviations from the norm, for example:
- in the thickness of the endometrium;
- size and shape of the body of the uterus, as well as its appendages;
- determine the presence of cysts, neoplasms, their location and structure.
Normally, according to ultrasound, the size of the uterus in women does not go beyond the permissible limits. Its contours are even, clear, the structure of the endometrium without any inclusions. Outwardly, the organ looks like a pear with an inclination forward. Some women are diagnosed with a backwardly tilted uterus. This does not mean that such a phenomenon is attributed to pathology. For a woman who does not plan a pregnancy, this position of the uterus does not threaten anything. Otherwise, there is a possibility that there may be difficulties with conception.
Before menopause, the normal uterus, according to ultrasound, has the following parameters:
- thickness - 30-40 mm;
- width - 46-64 mm;
- length - 45-70 mm.
After menopause, the size and thickness of the uterus decreases to 42 mm (length), 30 mm (thickness), 44 mm (width).
When planning pregnancy, many women monitor the condition of the endometrium. They need to know that depending on the day of the cycle, the indicators change from less to more. After the ultrasounduterus in the conclusion reflect information about the M-echo. What it is? This is the density of the endometrium. The inner layer of the uterus depends on the day of the cycle. At its beginning, from the first to the fourth day, the endometrial index is from 3 to 9 mm, from the fifth to the fifteenth day - up to 15 mm, from the sixteenth day until the end of the cycle - up to 20 mm.
As for the retrouterine space, closer to the middle of the cycle or after ovulation, fluid accumulation can be visualized there.
What is determined during diagnostics

When an ultrasound of the uterus is done, the state of its densest layer, the myometrium, is also assessed. Normally, in its structure, it should be homogeneous. Its uneven contours may indicate a possible pathology. If at the same time the structure is heterogeneous, then it is probably adenomyosis.
The position and size of the uterus can be used to judge some diseases, for example, if:
- contours uneven - tumor, cancer, fibroids;
- organ deviation from the norm - adhesive or inflammatory process;
- neoplasms are visualized inside - polyps, cysts, fibroids;
- endometrium is thicker than it should be at the time of the study - hyperplasia;
- an enlarged cervical canal or its structure is heterogeneous - an inflammatory process associated with a developing infection.
The pathology of the development of the uterus - hypoplasia, may vary in the nature of the location (bottom hypoplasia, tubes, cervical, mixed, vaginal).
These figures need to be compared with other studies,which may be required to make an accurate diagnosis.
By the size of the uterus and appendages, you can establish a disease such as polycystic ovaries. At the same time, multiple cysts are visualized on the latter, and the growth of fibrous tissue between them is noted. Polycystic disease is characterized by a decrease in the size of the organ, while the ovaries, on the contrary, are enlarged. During a general diagnosis, a hormonal failure is established.
As for various formations, it is worth noting the risk of developing polyps in the endometrium, which may not manifest themselves in any way. With ultrasound diagnostics, the doctor can detect uneven growth of the inner layer of the uterus, resulting in a diagnosis of endometrioid polyps.
Endometriosis

If during an ultrasound the doctor sees a seal in the endometrium, then this, as a rule, indicates the presence of endometriosis. At the same time, the heterogeneous structure of the inner layer of the reproductive organ is visualized on the screen, with cysts present in some of its areas. A deviation from the norm is fixed, the size of the uterus according to ultrasound, as a rule, is somewhat larger.
In order to exclude the development of a cancerous tumor, a smear is taken for cytology, a biopsy of the affected tissues. When making a diagnosis, the results of an ultrasound examination are also taken into account. If the existing changes can lead to the development of a tumor, then a second ultrasound examination is performed after some time. It will allow you to determine how the tumor develops and the rate of its growth.
Uterine fibroids

Thisa benign neoplasm that may not manifest itself for a long time. It is diagnosed in 40% of women worldwide. Only under certain circumstances can it develop into a cancerous tumor. When conducting an ultrasound of the uterus, the degree of growth of fibroids is diagnosed in the weeks of pregnancy. This is explained by the fact that on the monitor the doctor sees a small round formation, like a fetal egg. Up to 5-10 mm in size, it is diagnosed as a myomatous node. Usually its size increases towards the end of the menstrual cycle. Therefore, they are sent for ultrasound diagnostics immediately after menstruation.
According to how the uterus looks on ultrasound, the following options for the location of fibroids are distinguished: submucosal, intramural and subsurous.
It is noteworthy that the presence of a neoplasm in the organ cavity does not prevent the onset and normal course of pregnancy. However, its dimensions are monitored separately. Pay attention to how far the node is from the attachment site of the placenta. Since too close arrangement can disrupt the utero-placental exchange, worsen blood circulation between the mother and the fetus.
Too large fibroids can become an obstacle to the growth and movement of the fetus, affect its location in the uterus. As indications for childbirth, the need for a caesarean section may be added.
When examining a woman after childbirth, pay attention to the location of the fibroids, as it was noted that during the restoration of the previous size of the uterus, it changed its location.
Ultrasound examination during pregnancy

Safe and fast diagnostics allows you to determine the norm of the uterus by ultrasound at any stage of pregnancy. When it is not yet greatly enlarged (at the beginning of pregnancy), the presence of tumors and cysts in the region of the appendages is determined. Since closer to the second trimester, the uterus begins to grow rapidly and it becomes more difficult to visualize them.
With the help of ultrasound from the first weeks of pregnancy, you can monitor how the fetus develops, set the heartbeat, determine the condition of the amniotic fluid, the height of the uterine fundus and many other parameters. Prenatal diagnosis allows you to determine how the fetus is located inside (uterine or ectopic pregnancy, breech or head presentation). In order to identify genetic and congenital defects, screening studies are carried out in the second and third trimesters.
The uterus increases in size during pregnancy, so the parameters of the placenta are measured separately. Assess its thickness, the state of blood flow, the degree of maturity. Usually, if any pathologies or multiple pregnancies are detected, a photo is taken with an ultrasound of the uterus.
Diagnosis of the cervix
Special attention deserves the cervix, the rate of which is normal during pregnancy should be at least 3 cm, and she herself should be closed. If its dimensions in the process of carrying a baby become smaller, and the cervix opens slightly, which can be detected by visual inspection on the chair, then there is a risk of premature birth.
This item gets a lot of attention throughout pregnancy, especially among thosewomen who experienced miscarriage and premature birth. In case of deviation from the norm in the conclusion, according to the results of an ultrasound examination, a diagnosis of "isthmic-cervical insufficiency" is made.
Ectopic pregnancy on ultrasound

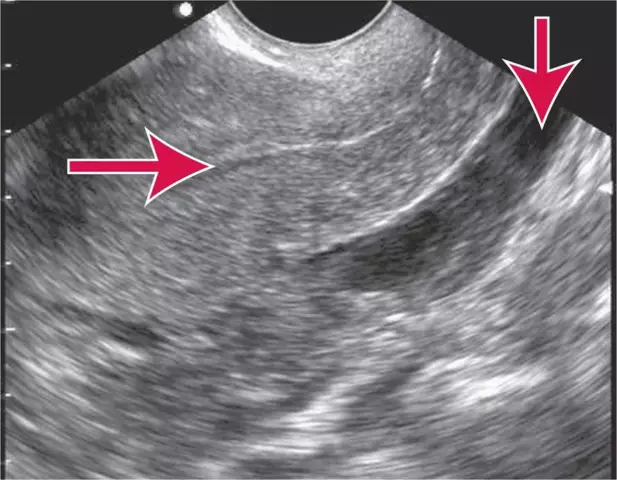
During an intravaginal examination of the vagina, an ectopic pregnancy can be diagnosed. When, according to the signs, it is, but the fetal egg is not visualized in the uterine cavity, the diagnostician pays attention to the appendages, the fallopian tubes. It is here, as a rule, that a fertilized egg “gets stuck” and develops.
In addition to the thickening in the area of the fallopian tube, a small blood clot is also visualized on the screen behind it. Having established an ectopic pregnancy at an early stage, it is possible to perform surgery and leave the tube intact. In the process of rehabilitation, a repeated ultrasound examination is performed, which helps to determine the degree of success of the manipulations performed.
Ectopic pregnancy, which at an early stage (up to 6 weeks) is visualized in the uterine cavity, leads to complications. But over time, it turns out that this is just a blood clot, which was mistaken for a fetal egg. In this case, you can miss the time for surgery, which leads to rupture of the fallopian tube. Therefore, the diagnosis of early pregnancy is carried out in several stages using additional methods, for example, a blood test for hCG.