- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
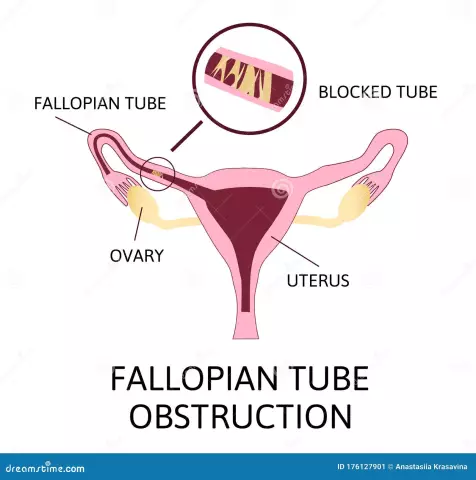
One of the necessary conditions for pregnancy is the normal patency of the fallopian (or fallopian) tubes in a woman. After all, it is through these channels that the fertilized egg enters the uterus. If the patency is impaired, then the woman is diagnosed with infertility. In case of partial obstruction, a life-threatening condition may occur - an ectopic pregnancy. To protect a woman from such problems and assess her chances of conceiving a child, the doctor prescribes an ultrasound of the patency of the fallopian tubes.

Survey summary
To assess the patency of the fallopian tubes, the patient is assigned an ultrasound of the patency of the fallopian tubes, or, in the language of physicians, hysterosalpingoscopy (HSG). This is a special diagnostic study, which, with the help of an injected contrast agent,allows you to explore the female genital area.
Unfortunately, conventional ultrasound is not able to fully provide information about tubal patency. That is why doctors resort to a special technique that detects unpleasant pathologies.
Ultrasound (HSG) of the fallopian tubes can be performed in two ways:
- transvaginally (insertion into the vagina);
- when using outdoor sensor.
This examination method is completely safe and very effective.

Indications for research
Any alarming signs, incomprehensible pains in the lower abdomen, the appearance of deviations in the cycle are serious reasons to go to the gynecologist for a consultation. If necessary, the doctor will prescribe a woman an ultrasound of the fallopian tubes for patency. However, the doctor issues such a referral only after a gynecological examination.
Ultrasound (HSG) of the fallopian tubes is recommended for women who have the following pathologies:
- disturbed menstrual cycle (irregularity or absence of periods);
- infertility;
- past sexually transmitted infections;
- constant pain discomfort in the lower abdomen;
- inflammation of the appendages.
In such conditions, the examination may be prescribed after the treatment. This allows you to determine the effectiveness of the prescribed therapy and assess the condition of the woman. Ultrasound of the patency of the fallopian tubes can be performed repeatedly. After all, such a study is painless and does not harm the femalehe alth.
Due dates
To get the most reliable clinical picture, you need to choose the right days. This is very important when an ultrasound is performed. Gynecology (which days are considered the most suitable, we will describe below) is a special branch of medicine that requires responsibility on the part of the doctor, because the he alth of not only the woman, but also her future offspring depends on his actions.

Doctors recommend conducting a study taking into account the following terms:
- The period from the 6th day of the cycle to the 21st.
- Some gynecologists advise to conduct an ultrasound before ovulation, from the 7th to the 12th day of the cycle.
Why are these terms considered the most optimal? Doctors say that during these periods the cervix is maximally expanded. The endometrium after menstruation is characterized by a minimum thickness. These features allow you to conduct the study as accurately as possible.
Preparing for the study
Ultrasound of the fallopian tubes for patency is a great chance to detect pathology at an early stage, start adequate therapy in a timely manner and completely get rid of the disease.
However, in order to correctly diagnose a woman's condition, it is necessary not only to choose the appropriate timing for the procedure. It is equally important to properly prepare for the study. The gynecologist will definitely tell about all the necessary measures.

The pre-survey phase usually includes:Events:
- Passing a smear on the microflora of the vagina. Such an analysis is valid for 21-45 days. Be sure to check with your doctor about the expiration date of the smear.
- A blood test for the following indicators: F-50 (for HIV), RW (for syphilis), hepatitis B, C. The results of these studies are considered valid for 6 months.
- Adherence to a special diet 3 days before the examination. During the event, it is necessary to exclude the presence of gases in the intestines. That is why it is important to adhere to a diet for 3 days aimed at reducing fermentation in the digestive tract. Give up flour, sweet, sour milk. Do not eat vegetables, fruits, carbonated drinks, legumes.
- Keeping your vagina clean. A week before the ultrasound, it is recommended to stop using vaginal sprays, suppositories, tablets. Avoid douching.
- Taking an antispasmodic. 20 minutes before the start of the procedure, the patient will be advised to use an antispasmodic drug (Spazmalgon, No-Shpa). Such a medication will provide relaxation of smooth muscles and prevent reflex contractions of the uterus. Sometimes such drugs are injected into a woman before the procedure.
Surveying
The procedure consists of several steps:
- Diagnosis of the fallopian tubes begins with a preliminary ultrasound monitoring of the state of the pelvic organs. Such a study is carried out in order to exclude the woman's pregnancy and the presence of inflammation.
- The patient sits comfortably in the gynecological chair. Disposablethe catheter is inserted intravaginally into the cervix. Through it, a contrast agent enters the organ cavity, preheated to a comfortable temperature (37 degrees). The solution fills the uterus and travels up the fallopian tubes. The contrast medium is then moved into the abdominal cavity.
- It is at the third stage that the analysis for the patency of the pipes begins. Free fluid localized in the pelvis indicates satisfactory patency. Much worse if the substance does not penetrate into the peritoneum. The liquid that has not left the limits of the pipes clearly indicates the obstruction of the channels. This study also allows you to determine the rate of advance of the contrast agent through the ducts.

Ultrasound with the use of a contrast agent makes it possible to assess the condition of the uterus and its structure:
- the shape and contour of the organ;
- presence of polyps and myoma formations;
- relief and thickness of the endometrium;
- development of an organ and pathology in its structure.
Study duration averages 25-30 minutes.
Survey results
During the procedure, a special sensor records the presence of fluid in the peritoneum. The doctor begins the examination with the uterus. Then determines the condition of the fallopian tubes. After that, if necessary, completes the examination with the study of the ovaries.
Ultrasound of the patency of the fallopian tubes reveals:
- congenital anomalies;
- fibroids, polyps, endometriosis, fibromas;
- adhesive processes (at the same time it clearly defineslocalization of pathology);
- pipe contours;
- location of the uterine canals.
Contraindications for testing
Ultrasound for the patency of the fallopian tubes is a fairly simple procedure. It does not imply invasive intervention and does not require complex preparation for implementation. But even such a simple examination has a number of contraindications.

Ultrasound is strictly prohibited:
- for uterine bleeding;
- gynecological diseases occurring in acute or chronic form;
- violations of the microflora of the vagina;
- pelvic inflammatory disease;
- pregnancy;
- tumors (benign, malignant) localized in the pelvis;
- infectious pathologies during an exacerbation.
Tubal patency test: research cost
How much does this examination cost women? Of course, depending on the chosen clinic, the cost of ultrasound for the patency of the fallopian tubes will also vary. The average price of the procedure is 5395 rubles.
Research Benefits
HSG has a number of advantages over other diagnostic methods for fallopian tube patency.
The main benefits of ultrasound are:
- The procedure does not require hospitalization.
- The injected liquid separates the spliced areas, washes off the derivative.
- During the study, many pathologies of the uterus are detected along the way.
- Promotes the egg.
- The patient does not need anesthesia.
- The study is carried out quickly enough, and the results are visible immediately.
- No need for peritoneal punctures.

Noticing the first alarming symptoms, do not put off a visit to the gynecologist. Be sure to seek the help of competent specialists who, if necessary, will recommend you an effective and safe ultrasound.