- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
At the moment, modern society is threatened by several epidemics at once, which threaten to turn into pandemics. These are diseases such as HIV, hepatitis B and C and, of course, tuberculosis. A high mortality rate and disabling consequences do not leave a person with a chance to fight the disease, and given that the diagnosis depends on the patients themselves, their trust in the doctor and their desire to be treated, then we have, to put it mildly, an unpleasant picture.
Definition
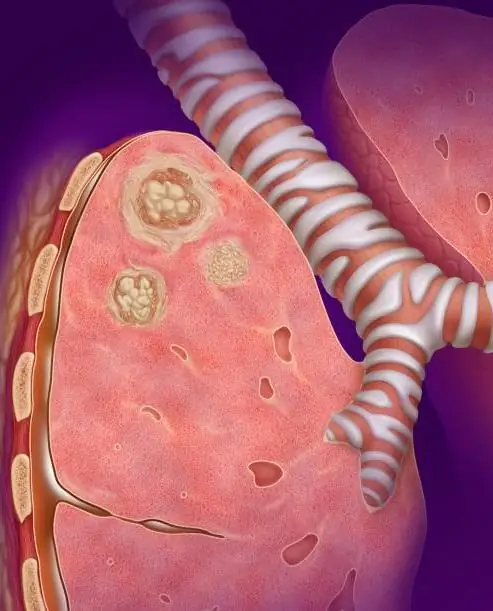
Caseous pneumonia is one of the forms of development of pulmonary tuberculosis. It is more malignant than ordinary pneumonia caused by coccal flora. And it is characterized by the predominance of necrotic processes in the lungs with the formation of cheesy masses instead of normal lung parenchyma. Over time, they undergo lysis, and large cavities remain in their place. Subsequently, they can either scar, which reduces the airiness of the lungs and, accordingly, the amount of incoming oxygen, or expand, pushing the parenchyma of the organ to the periphery. This process also negatively affects gas exchange and leads to the progression of exogenous hypoxia.
Classification
Depending on the area of damaged tissue, caseous pneumonia is divided into three subtypes:
- Lobarnaya. An independent form that captures the entire share entirely. Since the volume of damaged and necrotic tissue is large, a severe intoxication symptom predominates in patients. As a result, the lung melts and cavities form.
- Lobular form, or lobulitis. This is a complication of already existing tuberculosis. Unlike the previous one, it affects several lobes, causing severe poisoning with tissue decay products.
- Acinous. It is considered as a complication of miliary (loose) tuberculosis. Despite the fact that the acinus is the smallest part of the lung, the disease is extremely difficult to tolerate, since usually not single areas are affected, but the entire parenchyma of the organ.
Epidemiology

As noted above, tuberculosis is complicated by such a type of disease as caseous pneumonia. The history of the disease has more than one hundred years, and during this time people have not been able to come up with a treatment. Antibiotics that patients are taking now will become irrelevant in ten to twenty years, because the pathogen has time to develop resistance to this chemical effect.
The disease develops rapidly, the first symptoms appear fairly quickly after infection. Toxins produced by bacteria negatively affect the immune system, weakening it. The main contingent subject to caseous pneumonia are sociallydisadvantaged people. And not only because of the lack of basic hygiene, poor nutrition and living conditions, but also because of the refusal to treat the underlying pathology.
Disease development
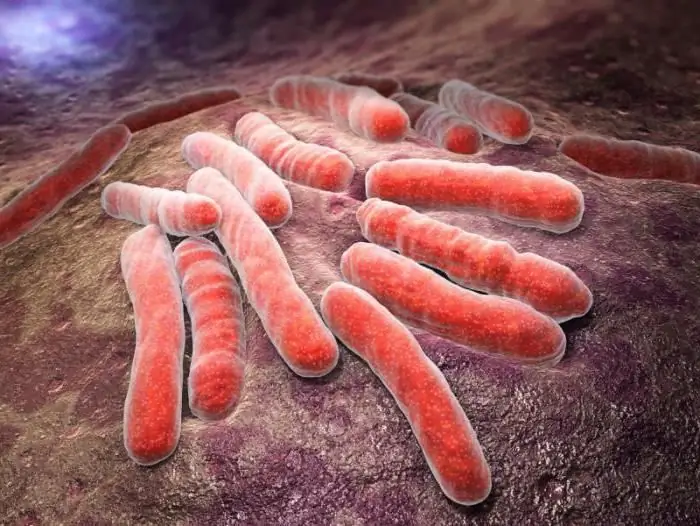
Due to the rapid division and growth of mycobacterium tuberculosis in the lungs, general and local immunity is suppressed. Microorganisms produce enzymes that have a toxic effect on cellular immunity, triggering the process of apoptosis (programmed cell death). Thus, after the accumulation of a certain critical mass of bacteria, the defense mechanisms of the human body begin to malfunction. A significant prevalence of the pathogen in the internal organs and the toxicity of drugs lead to a decrease in the function of the liver, adrenal glands, dystrophy of the heart muscle and damage to the nervous system.
Locally, against the background of a decrease in immunity, necrotic processes are observed in the lung parenchyma, multiple foci of inflammation with cheesy masses inside. Gradually, they are dissolved by the body's own enzymes, and caverns (cavities) appear in their place.
Symptoms
The clinical course of caseous pneumonia can have several scenarios:
- Pneumonic, i.e. similar to classic pneumonia - high fever (up to forty degrees), chills, wet cough, chest pain, severe shortness of breath.
- Influenza-like - catarrhal phenomena (runny nose, lacrimation, swelling of the larynx) prevail over intoxication. There is a slight fever, there may be a cough.
- Sepsis - very high temperature (up to forty-forty one degrees), intoxication, migraine, no cough.
At first, there are no alarming symptoms. Easy dry cough, rise in temperature at night, loss of appetite. They can last long enough until the cough turns from dry to wet, and viscous greenish sputum appears. By this time, the temperature is already subsiding, and respiratory failure, on the contrary, is increasing. The doctor may suspect that the patient has caseous pneumonia. The symptoms are non-specific, but in combination with tests and anamnesis of life, the diagnosis becomes clear.
Diagnosis
In addition to collecting an anamnesis of the disease and an anamnesis of life, the doctor must carefully examine the person, if possible, palpate his lymph nodes, listen to his breathing. But in order to make sure that his assumptions are correct, the doctor sends the patient to laboratory and instrumental studies:
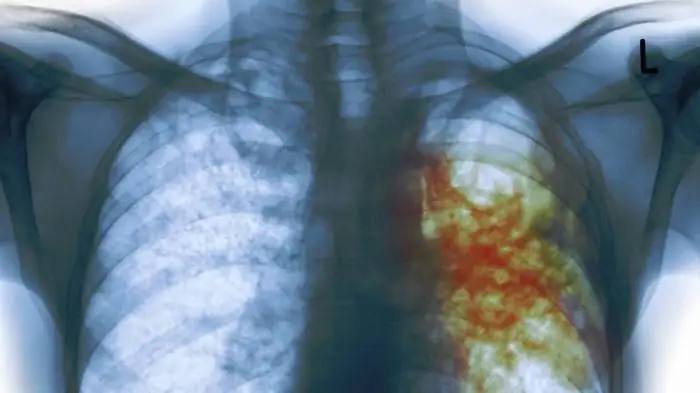
- Chest x-ray. Phthisiologists have discovered characteristic signs that are inherent in such a disease as caseous pneumonia. The photograph of the lungs above shows multiple foci of organ tissue melting.
- Mantoux test, or Diaskintest. A simple and relatively quick way to detect the presence of TB immunity. But it does not give a hundred percent guarantee of the development of the disease, and can be both false positive and false negative.
- Sputum microscopy. The patient is asked to collect sputum three days beforesterile jar. Then it is taken to the laboratory, where it is placed in a special Lowenstein-Jensen medium containing many nutrients necessary for the growth of bacteria. And only a week later it will be known whether a person highlights Koch's wand or not.
- It is obligatory to carry out standard tests for making a clinical diagnosis: complete blood count, urine, blood biochemistry, blood sugar, feces for the eggworm.
Differential Diagnosis

First of all, the doctor needs to make sure that the patient really has caseous pneumonia. Differential diagnosis in this case helps to exclude diseases that are clinically very similar to the pathology we are considering. And in the first row becomes the usual croupous, or pleuropneumonia. Their only difference will be in the nature of the necrotic masses and in the pathogen. The rest of the parameters are similar.
The second suggestion could be a pulmonary infarction. But it is enough to make an angiogram to exclude such a scenario. In addition, the patient must have a history of either trauma, or atherosclerosis, or the introduction of air and/or oily solutions into the bloodstream.
The third disease worth comparing with is lung gangrene. In the process of development of this pathology, there is a fever, severe intoxication, but there will be no cough and sputum.
Treatment

After caseous pneumonia is diagnosed, treatmentstart immediately. The person is transferred to a special TB hospital, where it is possible to observe a suitable bed rest and diet.
First, the doctor treats the acute condition, whether it be toxic shock or respiratory failure. For this, the patient is given infusions of sorbents and diuretics, and plasmapheresis is performed. Then comes the turn of active therapy, when antibiotics, antihypoxants, anticoagulants, hormones, interferon come into play. Specific therapy is the use of antibiotic regimens designed specifically for Mycobacterium tuberculosis.
Forecast

Caseous pneumonia is quite difficult to treat, so the consequences for life and he alth will most likely be irreversible. It is even possible to completely destroy the lung, which inevitably leads to respiratory failure.
Recommendations that phthisiatricians give to people with identified Koch's bacillus boil down to the fact that you should not start the disease. It is necessary to start treatment on time and complete it, but due to the low socialization of patients, as well as their living conditions, caseous pneumonia remains a frequent complication of tuberculosis. This is an epidemic that doctors these days are barely able to handle.






