- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2024-01-09 08:18.
- Last modified 2025-01-23 17:01.
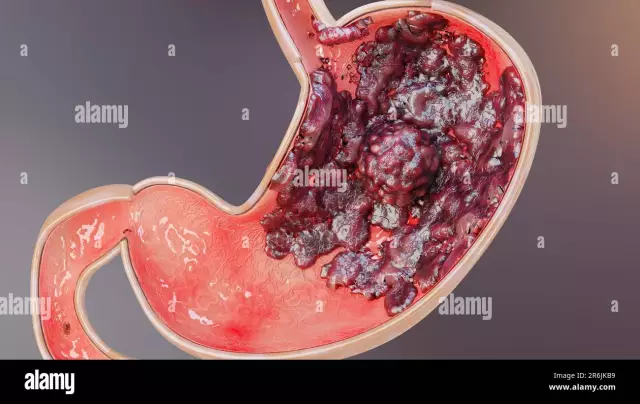
Myeloproliferative diseases, causes, symptoms, the diagnosis of which will be discussed below, are a group of conditions against which there is an increased production of platelets, leukocytes or erythrocytes in the bone marrow. There are six types of pathologies in total.

General information
Bone marrow normally produces stem (immature) cells. After a while, they mature, become full-fledged. A stem cell can be the source for the formation of two types of elements: cells of the lymphoid and myeloid series. Immature cells are the material for the formation of leukocytes. From the elements of the myeloid series are formed:
- Erythrocytes. They transport oxygen and other nutrients to organs and tissues.
- Leukocytes. These elements are responsible for resisting infectious and other pathologies.
- Platelets. These cells prevent bleeding and form clots.
Before transformation into erythrocytes, leukocytesor platelet stem cells need to go through several stages. If a myeloproliferative disease is present, then 1 or more types of formed cells are formed from a large amount of starting material. Usually, the pathology progresses rather slowly, as the excess of blood elements increases.
Classification
The type that a myeloproliferative disease can have depends on the number of red blood cells, platelets, or white blood cells. In some cases, there is an excess of elements of more than one type in the body. Pathologies are divided into:
- Chronic neutrophilic leukemia.
- Polycythemia vera.
- Chronic myelogenous leukemia.
- Essential thrombocytopenia.
- Idiopathic (chronic) myelofibrosis.
- Eosinophilic leukemia.

Stages of pathologies
Chronic myeloproliferative disease can transform into acute leukemia. This condition is characterized by an excess of white blood cells. Chronic myeloproliferative disease does not have a specific staging pattern. Therapeutic measures will depend on the type of pathology. In terms of transmission pathways, myeloproliferative disease can develop in one of three ways:
- Growing into other tissues. At the same time, the malignant neoplasm spreads to the surrounding he althy segments, affecting them.
- By the lymphogenic route. Myeloproliferative disease can invade the lymphatic system andvessels to spread to other tissues and organs.
- Hematogenous way. Malignant neoplasm cells invade capillaries and veins that feed tissues and organs.
When tumor cells spread, a new (secondary) neoplasm is likely to form. This process is called metastasis. Secondary, as well as primary neoplasms, are classified as one type of malignant tumor. For example, there is a spread of leukemic cells to the brain. Tumor elements are found in it. They refer to leukemia, not brain cancer.

Signs of pathology
How does myeloproliferative disease manifest itself? Symptoms of pathology are as follows:
- Weight loss, anorexia.
- Fatigue.
- Discomfort in the stomach and a feeling of rapid satiety with food. The latter is provoked by an enlarged spleen (splenomegaly).
- Predisposition to bleeding, bruising or thrombosis.
- Violation of consciousness.
- Joint pain, swelling caused by gouty arthritis.
- Tinnitus.
- Pain in the left upper quadrant of the abdomen and left shoulder due to inflammation or infarction of the spleen.

Examination
Myeloproliferative blood disease is diagnosed based on laboratory tests. The survey includes the followingEvents:
-
Examination of the patient. In this case, the specialist determines the general condition, reveals signs of pathology (swelling, for example), as well as manifestations that are not observed in a he althy person. The doctor also asks the patient about the lifestyle, previous diseases, bad habits, prescribed treatment.
-
Expanded UAC. Blood sampling is carried out to determine:
- the number of platelets and erythrocytes;
- the ratio and number of leukocytes;
- hemoglobin level;- the volume occupied by erythrocytes.
- Aspiration and bone marrow biopsy. During the procedure, a hollow thick needle is inserted into the sternum or ilium. These manipulations allow you to take samples of bone marrow and tissue, as well as blood. The material is examined under a microscope for the presence of pathological elements in it.
- Cytogenetic analysis. This procedure allows you to detect changes in chromosomes.

Chronic Myeloproliferative Disease Treatment
Today, there are several methods of treating pathology. One or another option is selected depending on the patient's condition and the manifestations that accompany the myeloproliferative disease. Treatment can be prescribed standard - proven by practice, or experimental. The second option is a study using various new tools.
Phlebotomy
This procedure involves taking blood from a vein. The material is then sent tobiochemical or general analysis. In some cases, phlebotomy is indicated for patients diagnosed with myeloproliferative disease. Treatment in this case is aimed at reducing the number of red blood cells.
Platelet Apheresis
This method is similar to the previous one. The difference is that excess platelets are eliminated with the help of special equipment. The patient takes blood, which is passed through the separator. It blocks platelets. The "purified" blood is returned to the patient.
Transfusion
This procedure is a blood transfusion. In this case, one element is replaced by another. In particular, the patient receives a transfusion of leukocytes, erythrocytes and platelets instead of his destroyed and damaged cells.

Chemotherapy
This method involves the use of cytotoxic drugs. Their action is aimed at destroying tumor cells or slowing down the growth of the neoplasm. With oral, intravenous or intramuscular use of drugs, their active components penetrate into the systemic circulation, destroying pathological elements. Such chemotherapy is called systemic. The regional technique is the introduction of funds into the spinal canal, the affected organ or the body cavity directly.
Radiation therapy
Treatment is carried out using X-ray or other high frequency radiation. Radiation therapy allows you to achieve absoluteelimination of tumor cells and slowing down the growth of neoplasms. In practice, two types of this treatment are used. External radiation therapy is the effect of the device, located next to the patient. With the internal method, needles, catheters, tubes are filled with radioactive substances, which are subsequently injected directly into the tumor or into the tissues located near it. Which method will be used by a specialist depends on the degree of malignancy of the process. Patients who are diagnosed with myeloproliferative blood disease are usually irradiated to the area of the spleen.

Chemotherapy with cell transplantation
This method of treatment consists in the use of drugs in high doses and the replacement of cells affected by antitumor effects with new ones. Immature elements are obtained from a donor or the patient himself and frozen. After the end of chemotherapy, the stored material is introduced into the body. The newly introduced cells begin to mature and activate the formation of new blood elements.
Recovery period
After treatment, the patient should visit the doctor regularly. To evaluate the effectiveness of therapy, it may be necessary to carry out a number of procedures used previously before the appointment. In accordance with the results obtained, a decision is made to continue, complete or change the treatment regimen. Some examinations should be repeated regularly even after the completion of the therapeutic course. They allow you to evaluateeffectiveness of interventions and timely detection of recurrence.