- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
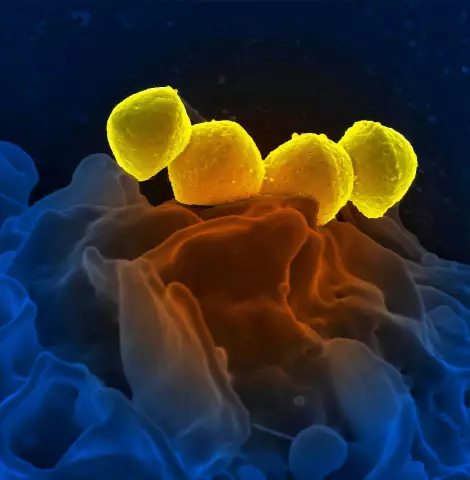
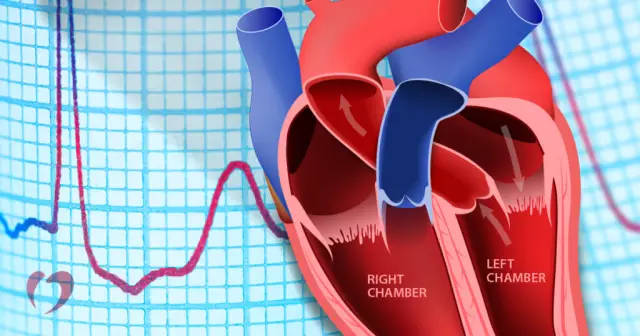
Atrioventricular blockade is a physiological violation of the transmission of nerve impulses through the conduction system of the heart from the ventricles to the atria. The seemingly complicated name comes from the Latin words atrium and ventriculus, which denote the atrium and ventricle, respectively.
About the heart, its structure and conducting system
The human heart, like many other living creatures related to mammals, consists of the right and left parts, each of which has an atrium and a ventricle. Blood from the whole body, namely from the systemic circulation, first enters the right atrium, and then into the right ventricle, then through the vessels to the lungs. Oxygen-enriched blood from the pulmonary circulation from the lungs flows into the left atrium, from which it enters the left ventricle, and from there it is transferred through the aorta to organs and tissues.
The blood flow in the heart ensures the functioning of its conducting system. It is thanks to her that the correct heartbeat occurs - the timely contraction of the atria and ventricles and the flow of blood through them. In violation of the transmission of nerve impulses between the atria andby the ventricles, the latter contract too slowly or out of time - after a long period of time after atrial contraction. As a result, the strength of the blood flow changes, it is not released into the blood vessels at the right time, there is a drop in pressure and other serious changes in the functioning of the cardiovascular system.
Why is AV block dangerous?
The degree of danger of atrioventricular blockade depends on its severity. Mild forms of conduction disturbances may be asymptomatic, moderate forms require clarification of the causes and treatment to prevent heart failure. With a complete blockade, instant death can occur from cardiac arrest. That is why the violation of nerve conduction in the heart cannot be ignored, even if at the moment there are no severe signs of the disease.

Classification by degree of AV block
AV heart block comes in several types and subtypes. By severity, they distinguish: first-degree AV block, often not accompanied by any external disturbances and in many cases is the norm, second-degree block, which, in turn, is divided into two subtypes: type 1 (Mobitz 1, or Wenckebach block) and type 2 (Mobitz 2), and third-degree blockade - a complete cessation of the transmission of nerve impulses from the atria to the ventricles.
1st degree AV block
1st degree AV block may be a normal physiological occurrence in young patients. It is often diagnosed in regularly trained athletes, and they are also consideredthe norm. With this blockage, a person usually does not have any noticeable symptoms that indicate heart problems. First-degree AV block in the absence of signs of disease usually does not require treatment, but it may be necessary in the presence of other abnormalities in the work of the heart. Also in this case, the doctor may prescribe repeated ECGs, daily ECG monitoring and additional studies, such as echocardiography (ultrasound of the heart). On an electrocardiogram, 1st-degree atrioventricular block appears as an increase in the interval between the P and R waves, while all P waves are normal and are always followed by QRS complexes.

2nd degree
AV-blockade of the 2nd degree is, as already described above, the first and second types. With the course according to the 1st variant (Mobitz 1), it can be asymptomatic and does not require treatment. In this case, the physiological basis for the occurrence of the block is usually a problem in the atrioventricular node. Second-degree Mobitz type 2 AV block is usually a consequence of pathology in the lower conduction system (His-Purkinje). As a rule, it proceeds with obvious symptoms and requires additional diagnosis and prompt treatment to prevent the development of a complete blockade with cardiac arrest.
AV blockade on ECG (second degree type 1) is characterized by a progressive increase in the PR interval, after which the QRS complex falls out and then - the restoration of a rhythm close to normal. Then everything repeats. This periodicity is called Samoilov's periodicals. Wenckebach. The second type of second-degree AV block on the ECG is characterized by permanent or spontaneous prolapse of the QRS complex, while prolongation of the PR interval, as in Mobitz type 1, does not occur.

3rd degree
3rd degree AV block can be congenital or acquired. It is characterized by the complete absence of impulses passing from the atria to the ventricles, and therefore is called a complete blockade. Since impulses are not conducted through the atrioventricular heart node, second-order pacemakers are activated to urgently support the work of the heart, i.e., the ventricle works according to its own rhythm, not associated with the atrial rhythm. All this causes severe disturbances in the functioning of the heart and the work of the cardiovascular system. Third-degree block requires prompt treatment as it can lead to death of the patient.
On an ECG, 3rd degree block looks like this: there is no connection between the P waves and the QRS complexes. They are recorded at the wrong time and with different frequencies, i.e. two unrelated rhythms are detected, one is atrial, the other is ventricular.
Causes of AV blockade
The most common causes of AV block disorder are increased vagal tone in athletes, sclerosis and fibrosis of the cardiac conduction system, valvular disease, myocarditis, myocardial infarction, electrolyte disturbances, and the use of certain drugs, such as cardiac glycosides (Digoxin,"Korglikon", "Strophanthin"), calcium channel blockers ("Amlodipine", "Verapamil", "Diltiazem", "Nifedipine", "Cinnarizine"), beta-blockers ("Bisoprolol", "Atenolol", "Carvedilol"). Complete blockade may be congenital. This pathology is often recorded in children whose mothers suffer from systemic lupus erythematosus. Another cause of third-degree blockade is called Lyme disease, or borreliosis.
Symptoms of AV block
Atrioventricular block of the 1st degree, as well as the 2nd degree block of the first type, is usually not accompanied by any symptoms. However, with the blockade of the Moritz 1 type, dizziness and fainting are observed in some cases. The second type of the second degree is manifested by the same signs, as well as clouding of consciousness, pain in the heart and a feeling of its stop, prolonged fainting. Symptoms of complete atrioventricular blockade are a decrease in heart rate, severe weakness, dizziness, blackouts, convulsions, loss of consciousness. A complete cardiac arrest with a fatal outcome may also occur.

Diagnosis of AV blockade
Diagnosis of atrioventricular blockade is carried out using electrocardiography. Often, AV blockade of the 2nd degree (as well as the 1st) is detected by chance during an ECG without complaints during a preventive medical examination. In other cases, the diagnosis is carried out in the presence of any symptoms that may beassociated with problems in the conduction system of the heart, such as dizziness, weakness, blackouts, fainting.
If a patient is diagnosed with AV block by ECG and there are indications for further examination, the cardiologist usually recommends 24-hour ECG monitoring. It is carried out using a Holter monitor, therefore it is also often referred to as Holter monitoring. Within 24 hours there is a constant continuous ECG recording, while a person leads a habitual and characteristic way of life - moves, eats, sleeps. The examination is non-invasive and causes almost no discomfort.
After the end of the electrocardiogram recording, the data from the monitor are analyzed with the issuance of an appropriate conclusion. The advantage of this diagnostic method, in comparison with the usual short ECG recording, is that it is possible to find out with what frequency blockades occur, during what period of the day they are recorded most often and at what level of patient activity.
Treatment
It is far from always that atrioventricular blockade of the first degree, as well as the second, requires medical intervention. With the 1st in therapeutic measures, as a rule, there is no need. Also, type 2 to type 1 (Moritz 1) usually does not receive therapy, although additional testing to detect associated heart problems may be recommended.
Treatment of AV block is necessary for second-degree Moritz type 2, as well as partial or complete third-degree block, because such a significant violationconduction can lead to sudden death. The main method of correcting the abnormal functioning of the heart is the installation of a patient with a pacemaker (EX), temporary or permanent. Specific drug therapy is also prescribed - "Atropine" and other drugs. Medicines are not able to cure a person with this disease and are usually used in the period before the implantation of the pacemaker.
Preparing for EKS installation
Preparation for pacemaker implantation includes, in addition to electrocardiography, echocardiography - an ultrasound of the heart. Echocardiography allows visualization of the wall, cavities and septa of the heart and detects any primary diseases that could be the cause of AV blockades, such as valvular pathology. If a cardiologist has detected heart problems during an ultrasound examination, concomitant therapy is carried out in parallel with the treatment of atrioventricular blockade. This is especially important in cases where it is these pathologies that are the cause of conduction disturbances. Standard clinical studies are also prescribed - blood and urine tests. If the patient has diseases of other organs and systems, appropriate diagnostic measures may be recommended in the preoperative period.

Former pacemaker implantation
Installation of a pacemaker with such a diagnosis as AV blockade is a planned surgical intervention. It can be carried out both under general anesthesia and under local anesthesia. surgeon through the subclavian veinconducts electrodes towards the heart, which are fixed there. The device itself is sewn under the skin using a special technique. The wound is stitched.
EX is an artificial pacemaker substitute that conducts impulses from the atria to the ventricles and normalizes the heartbeat. Due to periodic or continuous stimulation, the chambers contract in the correct order and at the correct interval, the heart fully performs its pumping function. The circulatory system does not experience congestion and sudden changes in pressure, and the risk of symptoms such as dizziness, loss of consciousness, and others that usually occur in patients diagnosed with AV blockade is significantly reduced, as is the risk of sudden death from arrest cardiac activity.

After surgery
The postoperative period, if there are no other he alth problems complicating it, is usually not accompanied by any serious restrictions. The patient is allowed to go home for 1-7 days, having previously done some research. Care of the wound in the area of the implanted body of the device is carried out according to the doctor's recommendations. Removal of sutures is necessary if they are applied with suture material that does not dissolve on its own. If during the installation of the pacemaker the wound was closed with a cosmetic suture, it does not need to be removed.
The first weeks after implantation of a pacemaker, it is recommended to avoid physical exertion, as well as protect the suture area (sports, if there are no contraindications, you can start afterseveral months after consulting a doctor). A follow-up consultation with a cardiologist is scheduled 1 month after the procedure. Then the check is carried out six months later and again a year later from the date of implantation, and then annually.
The time of the EKS depends on many factors. On average, this period is 7-10 years, and in children it is usually much less, which is associated, among other things, with the growth of the child's body. The control of the stimulator, as well as its programming for a particular patient, is carried out by a doctor. Checking the performance of the device must be carried out in a timely manner. Also, if necessary, the program is adjusted - the specified parameters of functioning. This may be necessary if the pacemaker is not doing its job: the heart rate is too low or too high and/or the patient is not feeling well. Also, other settings can be set by the doctor when a person’s lifestyle changes and there is insufficient stimulation, for example, during active sports.

The main reason for the failure of the EX is a decrease in battery capacity - its discharge. In such cases, the device must be replaced with a new one, and consultation with a cardiologist is required. The electrodes located in the cavity of the heart usually remain for life and do not require replacement if they work properly, enabling a person to live fully, despite heart problems.