- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-06-01 06:18.
The class of inflammation of soft tissues consists of separate nosological varieties of common etiopathogenesis. Pathological processes can be of a different nature and be of several types
The clinical picture of soft tissue inflammation, despite the variety of nosological types and localization of processes, has common symptoms for all of them. It is significant for the tactics of physiotherapy treatment and is primarily due to the presence of an inflammatory process. This is the formation of a painful infiltrate with soft tissue edema, hyperemia of the skin over it (with a slight depth of the process) and symptoms of local hyperthermia, an increase in overall body temperature. In case of purulent-necrotic inflammatory pathologies of soft tissues, a fluctuation symptom is characteristic, in which the general reaction increases in the form of an intoxication syndrome with a fever of purulent-resorptiveorigin.

The development of such a syndrome is mainly due to the pathogenicity of a particular infectious agent. Lymphadenitis and lymphangitis, being independent nosological varieties, often complicate the course of all inflammations in soft tissues. Inflammatory processes on the face are especially difficult and dangerous to he alth. At the same time, purulent foci sometimes open spontaneously.
Main symptoms
The main symptoms of soft tissue inflammation are:
- inflammatory;
- intoxication;
- pain;
- lymphostasis;
- trophic and metabolic disorders.
Varieties of the pathological process
The group of varieties of this disease includes:
Furunculosis is a purulent-necrotic inflammatory process of an acute nature, affecting the hair follicle and surrounding connective tissues. This pathology can be of a recurrent chronic nature and differ in the appearance of multiple boils on the body (at different stages of development).
Phlegmon - purulent diffuse inflammation of cellulose tissues. This pathology differs from an abscess in that the formation is delimited from nearby tissues by a specific pyogenic membrane. It has a tendency to spread through cell spaces. There is inflammation of the soft tissues of the leg.

It is very easy to get in everyday life. Various inflammations occur due to broken knees, abrasions, scratches. Microbes penetrate the soft tissues of the legs through:
- skin scratching;
- fungal diseases;
- diabetic ulcers;
- varicose veins;
- injection in unsanitary conditions;
- injuries and wounds;
- drift of microflora with blood or lymph from primary inflammatory foci.
For the same reasons, inflammation of the soft tissues of the hand may occur.
Carbuncle is a purulent-necrotic inflammatory process of an acute form, affecting several sebaceous glands and hair follicles and spreading to the skin and subcutaneous tissue.
Bursitis is an inflammatory pathology of synovial bags, which is accompanied by the accumulation of exudate in their cavities. Mastitis is an inflammation of the parenchyma and interstitium of the mammary gland. There is inflammation of the soft tissues of the joints.
Abscess - a limited accumulation of purulent masses in various organs and tissues.
Panaritium - inflammation of the soft tissues of the finger. This category includes almost all varieties of panaritium, except for bone, articular and pandactylitis, in which dense tissue formations and structures of the finger are subject to damage.
Paraproctitis is an inflammation of the perirectal fiber, which is caused by the presence of an infectious focus in the wall of the rectum.
Lymphadenitis is an inflammatory process that develops in the lymph nodes and occurs in most cases secondarily. It is a complication of various pyoinflammatory pathologies and specific infections.
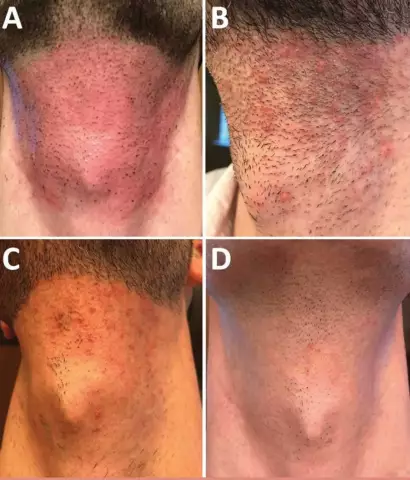
Hydradenitis - inflammatorythe process occurring in the apocrine sweat glands of a purulent nature.
Reasons
The causative agents of soft tissue inflammation are pathogenic bacteria, in most cases - various types of staphylococci. Sometimes there are pathogens such as E. coli and anaerobic infection. Their penetration into tissues occurs with wound injuries, microtraumas (during scratching, injections, carried out in violation of antiseptic rules). The introduction of pathogenic microflora by lymphogenous, hematogenous and contact routes from primary infectious foci is possible. Inflammation develops through proliferative and alterative-exudative phases with outcome in sclerotic changes and reparative regeneration.

Symptoms of the pathological process at different stages
This disease is a process that occurs in three main stages. The first stage of the pathological phenomenon, as a rule, occurs abruptly and is asymptomatic.
Initially, inflammation causes alteration - a violation of circulation in small vessels, which is associated with the transformation or damage to tissue structures. The narrowing of capillaries during the inflammatory process in soft tissues, in turn, provokes malnutrition, that is, weakening and a decrease in muscle volume. If at this stage the pathological phenomena associated with inflammation are not eliminated, it tends to move into the second - exudation, which is a pronounced swelling, and later - into the third.
In the second stage
On the second stageinflammatory disorders in soft tissues, pain occurs. The tissues are literally bursting from the fluid that has collected in them, and they are forced to signal this through pain.
So, the source of pain in the body during inflammation is damaged muscle fibers, and through neuromuscular connections information about these disorders enters the nervous system. Therefore, it is extremely important to adequately interpret the pain instead of taking painkillers with the development of such a pathological process in soft tissues, as happens in the vast majority of cases. As a result of all that is happening, there is a rupture of neuromuscular connections, the muscle stops transmitting information about its damage to the motor neuron. Under the influence of painkillers, muscle atrophy and tendon contracture develops.
Third stage of inflammation
The third stage of the inflammatory process is called proliferation and is the resorption of soft tissue edema. This can happen spontaneously, which can be facilitated by special exercises - the creation of natural drainage.

Diagnosis
The occurrence of purulent-inflammatory processes is characterized by a wide variety of clinical manifestations. According to medical research, 40-50% of patients are referred for inpatient treatment.
Efficiency of therapy of patients with purulent-inflammatory diseases of soft tissues depends on the timely diagnosis of such pathologies. Correctlythe diagnosis allows effective treatment and return to normal life.
Diagnosis in the initial phase can be significantly difficult, since using common methods it is difficult to determine the nature of disorders in bone tissue, where the process often spreads from soft.
What is the history?
During the diagnostic study, the surgeon or traumatologist pays attention to the presence in the patient's history of indications of the development of inflammatory symptoms after trauma, wounds or injections. For example, a superficially localized soft tissue abscess is easily identified by examination of the area. Deeper pathological processes require ultrasound examinations and diagnostic punctures. After the puncture, the obtained biological material is subjected to bacteriological studies to determine the sensitivity of purulent microflora to antibacterial drugs.
In addition, the list of basic diagnostic measures includes such as X-ray examination of the affected area and PCR diagnostics for tuberculosis. Background pathologies of the patient are also diagnosed, for which it may be necessary to consult other specialists: a gastroenterologist, an otolaryngologist, an endocrinologist.
Treatment of pathology
Common for all types of inflammation of soft tissues, the methods of treatment are anti-inflammatory (including antibacterial) and detoxification. It is also necessary to have a restorative treatment prescribed against the background of an operativetherapy.
Antibiotics are used for inflammation of soft tissues, most often penicillins ("Amoxicillin", for example), the course of treatment is 10 days, up to four times a day, 250-500 mg. If the patient is allergic to penicillin, macrolides ("Erythromycin", "Clarithromycin") for 10 days, 250-500 mg, but twice a day, will be no less effective.

In addition, antibiotics for external use are used - ointments "Mafenid", "Levomekol", "Levosin". Recovery occurs in 1-2 weeks.
The course of purulent inflammation of soft tissues and methods of its postoperative treatment or spontaneous opening of the focus of inflammation are inextricably linked with the treatment of wounds and wound infections.
Conservative treatment
Conservative treatment includes physical methods that are carried out in the presence of an infiltrate or a small amount of pus, as well as in the absence of a transition process to tendons, joints, organ tissues, serous cavities. This is also advisable in the absence of symptoms of intoxication, since in these cases immediate surgical intervention is required, regardless of the degree of the pathological process.
What else is used in the treatment of soft tissue inflammation?
Physiotherapy
At all stages of the inflammatory process in soft tissues, the fundamental goal of physiotherapy is the sanitation of the infectious focus of infection (bactericidal methods), the elimination of the directly inflammatoryprocess. At the stage of infiltration without symptoms of purulent fusion of tissue or with a small amount of pus (without fluctuation, in the absence of a general reaction), the goal of physiotherapy will be the reverse development of the inflammatory process with resorption of the infiltrate and the elimination of edema (anti-inflammatory methods of therapy), relief of pain (analgesic methods).

In cases of delayed formation of an abscess, physiotherapy is prescribed in order to soften the infiltrate and accelerate the removal of necrotic masses. Physiotherapy is also used to enhance the processes of reparative regeneration, increase the level of nonspecific resistance (immunostimulating methods) and reduce ischemia (antihypoxic methods of treatment). Helps to quickly relieve inflammation of soft tissues.
Methods
These goals are realized by the following methods of physiotherapy:
- bactericidal method of therapy - electrophoresis of antibacterial drugs;
- anti-inflammatory techniques - electrophoresis (solution) of calcium chloride, UHF therapy, low-intensity CMW therapy, SUV irradiation;
- immunostimulating techniques: LOC, DUV irradiation, high-frequency magnetotherapy, general SUV irradiation, heliotherapy, electrophoresis of immunomodulators;
- necrolytic methods: high-intensity UHF and microwave therapy, irradiation.
- analgesic therapies: SUF - diadynamic and amplipulse therapy, electrophoresis with local anesthetic drugs, irradiation;
- reparative-regenerativetechniques: microwave therapy, laser therapy, high-frequency and low-frequency magnetotherapy, ozokerite therapy.
- fibromodulating techniques: phonophoresis with defibrosing drugs, ultrasound therapy, pelotherapy.
- vasodilators: electrophoresis with vasodilators, infrared irradiation;
- antihypoxic technique - oxygen barotherapy;
- detoxification - AUFOK.
Consequences
The consequences of this pathological process depend on its localization, timeliness and adequacy of the treatment. This type of soft tissue inflammation, such as an abscess of the subcutaneous tissue, in most cases ends in absolute recovery. With a brain abscess, the prognosis is very serious, death is observed in 10% of cases. Any other inflammation of the soft tissues also disappears with the disappearance of all symptoms, if you choose the right methods of treatment. Furunculosis and carbuncles, for example, are treated for a long time, especially if the pathology has become chronic. However, these diseases also tend to be cured.

Prevention of pathology
Prevention of the development of diseases of this nature is aimed at preventing the entry of pathogenic pyogenic microflora into the body and includes the following measures: adherence to antiseptics during medical procedures (for example, injections) that are accompanied by damage to the skin; timely implementation of primary treatment of woundedsurfaces; rehabilitation of chronic foci of infection; increased immunity; hygiene.