- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
Surgical infection is a complex of diseases manifested as a result of the penetration of pathologically dangerous bacteria into the tissues after the operation. For such phenomena, the occurrence of a focus of inflammation and reactions of the body to foreign microorganisms is characteristic. Traditionally, modern medicine has used antibiotic therapy as a treatment and prevention of surgical infection. Nevertheless, there are situations when surgical intervention is indispensable, since many diseases are accompanied by purulent-septic complications.

Classification of surgical infection
Postoperative pathological process, which has an infectious nature of development, is divided into acute and chronic. The first category includes:
- purulent;
- rotten;
- anaerobic;
- specific (such as tetanus, anthrax and diphtheria) infections.
The second category is:
- non-specific;
- specific(such as Mycobacterium tuberculosis, syphilis bacteria, actinomycosis, etc.).
There are several classifications for surgical diseases accompanied by purulent processes.
Etiological signs
In addition, surgical infections are pathologies that are divided according to etiological characteristics, namely:
By source of infection:
- endogenous;
- exogenous.
By type of infectious agent:
- staphylococcal;
- streptococcal;
- pneumococcal;
- colibacillary;
- gonococcal;
- anaerobic non-spore-forming;
- clostridial anaerobic;
- mixed type.
By type of origin there are surgical infections:
- hospital;
- out-of-hospital.
By type of pathology:
- diseases of infectious and surgical origin;
- complications of infectious-surgical diseases;
- postoperative infectious complications;
- complications of an infectious nature in closed and open injuries.
According to the clinical course:
- in a sharp form;
- in chronic.
According to the localization, various types of surgical infection can affect:
- skin and subcutaneous tissue;
- the brain and its membranes;
- neck structure;
- chest, pleural cavity, lungs;
- mediastinal organs complex;
- peritoneum and abdominal organs;
- small organspelvis;
- bones and joints.

Main pathogens
Surgical infection is, first of all, pathogens that cause a specific and non-specific course. Despite the wide variety of diseases caused by infectious pathogenesis, they have much in common.
Non-specific infection
Most often occurs when some types of pathogens enter the tissues of the body. In this case, the responses of the body, despite the differences in the pathogen, will be similar, i.e. non-specific. In practice, such reactions are called purulent-inflammatory process. They can be caused by gram-positive and gram-negative, aerobic and anaerobic bacteria and pathogenic fungi. The most common pathogens that cause non-specific surgical infections are:
- Staphilicoccus aureus (Staphylococci) is a common microorganism that provokes the development of purulent-inflammatory processes. There are three varieties: golden, epidermal, saprophytic. The first variety is the most dangerous and belongs to pathogenic microorganisms. Epidermal, saprophytic are non-pathogenic pathogens, but in recent years they have been increasingly found in purulent-inflammatory diseases.
- Pseudomonas aeruginosa (Pseudomonas aeruginosa) - is normally determined on the skin and rarely causes purulent inflammation itself, but easily joins the emerging pathological microflora. When it enters the focus of infection, the inflammatorythe process is being delayed as Pseudomonas aeruginosa is resistant to many antibiotics.
- Eisherichia coli (E. coli) causes purulent-inflammatory pathologies of abdominal tissues (appendicitis, cholecystitis, peritonitis, abscesses, etc.).
- Enterococcus (Enterococci) - gram-positive cocci present in the composition of the microflora of the digestive system. In the presence of suitable conditions, they cause purulent processes.
- Enterobacter (enterobacteria) - just like enterococci, live in the intestinal system. They can provoke a purulent-inflammatory pathological process.
- Streptococcus (Streptococcus) - there are about 20 species of this microorganism. When infected, they cause severe intoxication and a protracted inflammatory process.
- Proteus vulgaris (Proteus) are Gram-negative rods normally found in the human mouth and intestines. They are a dangerous nosocomial surgical infection. Under suitable conditions and in tandem with other pathogenic pathogens, they provoke the development of severe purulent inflammation. Resistant to many antibiotics.
- Pneumococcus (Pneumococcus) - present in the microflora of the upper respiratory tract and nasopharynx. Contributes to the development of pneumococcal peritonitis, abscess of the lung and brain.
- Bacteria belonging to the group of nonfermenters. They represent a whole group of heterogeneous aerobic and anaerobic surgical infections. They have a low pathogenicity, however, under suitable conditions, they provoke putrefactive inflammations.
Purulent diseases can be caused by onepathogen (monoinfection) or several types of infections at once (mixed infection), forming a microbial association.
Cases when the inflammatory process is caused by several pathogens that exist in the same habitat (for example, aerobic) are called polyinfection. If microorganisms of different groups participate in the inflammatory process, then this is a mixed infection.

Surgical specific infection
In the first case, the pathological process is caused by certain microorganisms and leads to the appearance of foci of inflammation, characteristic only for these bacteria. These include: fungal bacteria, actinomycetes, spirochetes, corynobacteria diphtheria, anthrax bacteria.
Pathogenesis
The development of surgical infectious diseases is determined by three main factors:
- Type of pathogenic microorganism and its properties.
- Bacterial entry point (entrance gate).
- The reaction of the body to the penetration of infection.
Determination of the properties of a pathogenic microorganism involves the detection of its virulence (pathogenicity), which is estimated by the minimum dose of bacteria that provoke the development of infection. These characteristics depend on their invasiveness (the ability to overcome protective barriers and penetrate tissues) and toxigenicity (the ability to produce toxins that damage body tissues).

Properties of pathogenic microorganisms
Of course, depending on the varietystrain and the presence of other pathogens, the pathogenic properties of the pathogen may vary. Therefore, monoinfections are much easier and easier to treat.
Surgical infections are greatly aggravated if they are accompanied by secondary diseases, which often increase the activity of the primary pathogen. The quantitative factor is also important: the more pathogenic microorganisms have penetrated the tissues, the higher the likelihood of a purulent-inflammatory disease.

Entrance Gate
The first stage of the beginning of the infectious process is the penetration of the pathogen into the tissues. This phenomenon is called infection and can be exogenous (pathogenic microorganisms penetrate tissues from the outside, forming the primary focus of infection) and endogenous (activation of microbes already present in the body that previously did not pose a threat).
The skin and mucous membranes of the body are a barrier to infection. In cases of damage to their integrity or violation of the local defense mechanisms of the body, optimal conditions appear for the entry of pathogenic microflora. The entrance gate can be the ducts of sweat, sebaceous or mammary glands.
However, such an introduction does not always provoke an infectious process, since in most cases the bacteria die as a result of the action of immunity. Therefore, the likelihood of developing a pathogenic process depends on the location of the general surgical infection and the availability of favorable conditions.
The state of the immunesystems
The general condition of the body often plays an important role. With a small infection with weak pathogenic indicators, with good protective reactions of the body, the pathological process can be quickly suppressed or not develop at all.
The general protective reaction is determined by non-specific reactivity (depends on individual resistance, genetic factors, saturation of tissues with essential trace elements) and the general state of immunity.

Specific mechanisms
Each organism has the ability to produce its own antibacterial substances that protect it from the effects of invading pathogens. Immune protection is provided by the production of antibodies of the humoral and cellular type. These substances in the body begin to be produced as a result of exposure to toxins and enzymes of pathogens, as well as their metabolic products and decay products of their own tissues.
Which reduces protection
In some cases, an organism attacked by pathogenic bacteria may have some functional disorders characteristic of comorbidities. This leads to the impossibility of implementing milestones of protective reactions, which creates favorable conditions for the development of infection.
Factors that affect the likelihood of developing an infectious disease include:
- Gender of the patient. The female body has more pronounced protective reactions, therefore it is more resistant to infectious diseases.
- Age group. From infectious diseases more oftenchildren and older people suffer.
- Chronic fatigue.
- Poor nutrition and lack of vitamins. Nutrient deficiencies significantly weaken the overall state of the immune system.
- Anemia. This disease significantly weakens the protective properties of the body, while in infectious diseases anemia can rapidly develop against the background of the disease.
- Hypoglobulinemia, hypovolemia and a number of other pathologies. Contribute to the development of infection.
Favor the development of the disease and many other conditions of the body, in which there are blood flow disorders (for example, diseases of the cardiovascular system), immunodeficiency diseases (for example, diabetes mellitus).
The course of the pathogenic process
The infectious process is divided into stages: incubation, peak and recovery. During each of these periods, various processes occur both in the focus of inflammation and in the body as a whole. Changes that occur during the infectious process are divided into protective (resistance of the body) and pathological (destructive effects of infection).
The starting point of the incubation stage is considered to be the moment when the pathogenic environment enters the body, however, the clinical manifestations of this process may appear only after some time (on average, about 6 hours).
The stage of the peak of infection is the period from the end of the incubation stage to a complete cure. It manifests itself with a characteristic picture for a characteristic pathogen in combination with the protective ability of the body.
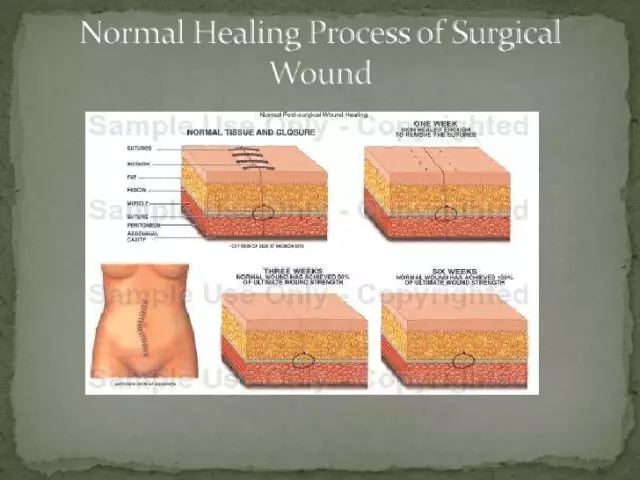
Reconvalescence(recovery) occurs after the provision of appropriate antibacterial care for surgical infection. As a result of adequate therapy, the activity of the infectious process subsides, the body recovers, eliminating the consequences and damage caused by the disease.

Symptoms
General symptoms in surgical infection manifest themselves depending on the duration of the course of the disease and its stage. The incubation period is usually asymptomatic, only some infectious diseases may present with headache, weakness, etc.
During the height of infection, clinical manifestations manifest themselves as endogenous intoxication syndrome, as they are caused by exposure to microbial toxins and decay products of body tissues. Signs of this process are manifested in the form of: malaise, lethargy, weakness, insomnia, headache, fever, etc.
The clinical picture of the manifested symptoms is more pronounced in the purulent-necrotic stage than in the serous-infiltrative one. In addition, the symptoms depend on the severity of intoxication.