- Author Curtis Blomfield [email protected].
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
Each of us has experienced inflammation of one kind or another. And if its serious forms, such as pneumonia or colitis, happen in special cases, then such minor troubles as a cut or abrasion are commonplace. Many do not pay attention to them at all. But even the most minor injuries can cause exudative inflammation. In fact, this is such a state of the affected area, in which specific fluids collect in it, and then seep through the walls of the capillaries to the outside. This process is quite complex, based on the laws of hydrodynamics and can lead to complications in the course of the disease. In this article, we will analyze in detail what causes exudative inflammation causes. We will also consider the types (outcomes for each of them are unequal) of this kind of inflammatory processes, and along the way we will explain what they depend on, how they proceed, what treatment they require.
Is inflammation good or bad?
Many will say that, of course, inflammation is evil, because itis an integral part of almost any disease and brings suffering to a person. But in fact, in the process of evolution, our body for many years developed the mechanisms of inflammatory processes in itself so that they would help to survive the harmful effects, which are called irritants in medicine. They can be viruses, bacteria, any skin wounds, chemicals (for example, poisons, toxins), adverse environmental factors. Exudative inflammation should protect us from the pathological activity of all these irritants. What it is? If you do not go into details, it is quite simple to explain it. Any irritant, once in the human body, damages its cells. This is called an alteration. It starts the inflammatory process. Its symptoms, depending on the type of irritant and the place of its introduction, may differ. Among the common ones are:
- rise in temperature either throughout the body or only in the damaged area;
- swelling of the affected area;
- soreness;
- redness of the injured area.

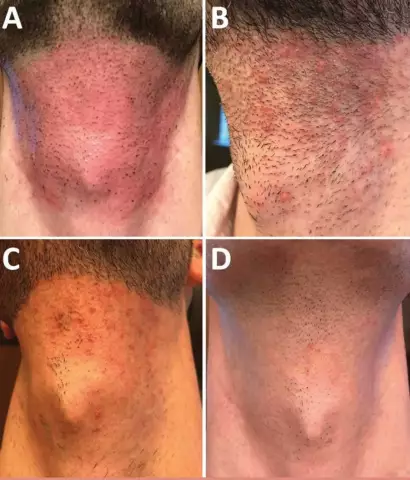
These are the main signs by which you can understand that exudative inflammation has already begun. The photo above clearly demonstrates the manifestation of symptoms - redness, swelling.
At some stage of the inflammatory process, fluid (exudate) begins to accumulate in the vessels. When they penetrate through the walls of the capillaries into the intercellular space, the inflammation becomes exudative. At first glance, this seems to be an aggravation of the problem. But in fact the way outexudate, or, as doctors say, exudation, is also needed. Thanks to it, very important substances enter the tissues from the capillaries - immunoglobulins, kinins, plasma enzymes, leukocytes, which immediately rush to the focus of inflammation in order to eliminate irritants and heal damaged areas there.
Exudation process
Explaining what exudative inflammation is, pathological anatomy (a discipline that studies pathological processes) pays special attention to the process of exudation, the "culprit" of this type of inflammation. It consists of three steps:
- There was an alteration. She launched special organic compounds - inflammatory mediators (kinins, histamines, serotonins, lymphokines and others). Under their influence, the channels of microvessels began to expand, and as a result, the permeability of the walls of blood vessels increased.
- In wider sections of the channels, the blood flow began to move more intensively. There was a so-called hyperemia, which, in turn, led to an increase in blood (hydrodynamic) pressure in the vessels.
- Under the pressure of fluid from microvessels, exudate began to seep into the tissue through enlarged interendothelial gaps and pores, sometimes reaching the size of tubules. The particles that make it up moved to the site of inflammation.

Types of exudates
It is more correct to call the exudate fluids leaving the vessels into the tissues, and the same fluids released in the cavity - effusion. But in medicine, these two concepts are often combined. The exudative type of inflammation is determined by the composition of the secret, which can be:
- serous;
- fibrous;
- purulent;
- rotten;
- hemorrhagic;
- slimy;
- chile;
- chyle-like;
- pseudochile;
- cholesterol;
- neutrophilic;
- eosinophilic;
- lymphocytic;
- mononuclear;
- mixed.
Let's take a closer look at the most common types of exudative inflammation, its causes and symptoms.
Form of serous exudative inflammation
In the human body, the peritoneum, pleura, pericardium are covered with serous membranes, so named from the Latin word "serum", which means "serum", because they produce and absorb fluids that resemble blood serum or are formed from it. The serous membranes in the normal state are smooth, almost transparent, very elastic. When exudative inflammation begins, they become rough and cloudy, and serous exudate appears in tissues and organs. It contains proteins (more than 2%), lymphocytes, leukocytes, epithelial cells.
Exudative inflammation can be caused by:
- injuries of various etiologies (violations of the integrity of the skin, burns, insect bites, frostbite);
- intoxication;
- viral and bacterial infections (tuberculosis, meningitis, herpes, chickenpox and others);
- allergy.
Serous exudate helps to remove toxins and irritants from the focus of inflammation. Along with its positive features, there are also negative ones. So, if serous exudative inflammation occurs in the lung parenchyma, respiratory failure may develop, in the pericardium - heart failure, in the meninges - cerebral edema, in the kidneys - renal failure, in the skin under the epidermis - exfoliation of it from the dermis and the formation of serous blisters. Each disease has its own symptoms. Of the general ones, one can distinguish a rise in temperature and pain. Despite the seemingly very dangerous pathology, the prognosis in the vast majority of cases is favorable, as the exudate resolves without leaving traces, and the serous membranes are restored.

Fibrous inflammation
As noted above, all types of exudative inflammation are determined by the composition of the secret released from the microvessels. So, fibrous exudate is obtained when, under the influence of inflammatory stimuli (trauma, infection), an increased amount of fibrinogen protein is formed. Normally, an adult should have 2-4 g / l. In damaged tissues, this substance turns into fibrin. This is also a protein that has a fibrous structure and forms the basis of blood clots. In addition, in the fibrous exudate there are leukocytes, macrophages, monocytes. At some stage of inflammation, necrosis of the tissues affected by the irritant develops. They are impregnated with fibrous exudate, as a result of which a fibrous film forms on their surface. Microbes actively develop under it, which complicates the course of the disease. dependingdiphtheria and croupous fibrous exudative inflammation are distinguished from the localization of the film and from its features. Pathological anatomy describes their differences as follows:
- Diphtheria inflammation can occur in those organs that are covered with a multi-layered membrane - in the pharynx, uterus, vagina, bladder, gastrointestinal tract. In this case, a thick fibrous film is formed, as if ingrown into the shell of the organs. Therefore, it is difficult to remove, and leaves ulcers behind. Over time, they heal, but scars may remain. There is another evil - under this film, microbes multiply most actively, as a result of which the patient has a high intoxication with the products of their vital activity. The best-known disease of this type of inflammation is diphtheria.
- Croupous inflammation is formed on mucous organs covered with a single layer: in the bronchi, peritoneum, trachea, pericardium. In this case, the fibrous film turns out to be thin, easily removed, without significant defects in the mucous membranes. However, in some cases, it can create serious problems, for example, if the trachea becomes inflamed, it can make it difficult for air to enter the lungs.

Exudative purulent inflammation
This pathology is observed when the exudate is pus - a viscous greenish-yellow mass, in most cases with a characteristic odor. Its composition is approximately the following: leukocytes, most of which are destroyed, albumins, fibrin threads, enzymes of microbial origin, cholesterol, fats, DNA fragments, lecithin,globulins. These substances form purulent serum. In addition to it, purulent exudate contains tissue detritus, live and / or degenerated microorganisms, purulent bodies. Purulent inflammation can occur in any organs. The “culprits” of suppuration are most often pyogenic bacteria (various cocci, Escherichia coli, Proteus), as well as Candida, Shigella, Salmonella, Brucella. Forms of exudative inflammation of a purulent nature are as follows:
- Abscess. It is a focus with a barrier capsule that prevents pus from entering neighboring tissues. Purulent exudate accumulates in the cavity of the focus, entering there through the capillaries of the barrier capsule.
- Phlegmon. With this form, there are no clear boundaries at the focus of inflammation, and purulent exudate spreads into neighboring tissues and cavities. Such a picture can be observed in the subcutaneous layers, for example, in adipose tissue, in the retroperitoneal and pararenal zones, wherever the morphological structure of tissues allows pus to go beyond the focus of inflammation.
- Empyema. This form is similar to an abscess and is observed in cavities, next to which there is a focus of inflammation.
If there are many degenerative neutrophils in the pus, the exudate is called purulent neutrophilic. In general, the role of neutrophils is to destroy bacteria and fungi. They, like brave guards, are the very first to rush at the enemies that have penetrated our body. Therefore, at the initial stage of inflammation, most neutrophils are intact, undestroyed, and the exudate is called micropurulent. As the disease progresses, leukocytes are destroyed, and in pusmost of them are already degenerated.
If putrefactive microorganisms (in most cases, anaerobic bacteria) get into the inflammatory focus, the purulent exudate develops into putrefactive. It has a characteristic odor and color and contributes to the decomposition of tissues. This is fraught with high intoxication of the body and has a very unfavorable outcome.
Treatment of purulent inflammation is based on the use of antibiotics and ensuring the outflow of secretions from the focus. Sometimes this requires surgery. The prevention of such inflammation is the disinfection of wounds. Treatment of this pathology can have a favorable outcome only with intensive chemotherapy with simultaneous surgical removal of rotting fragments.

Hemorrhagic inflammation
In some very dangerous diseases, such as anthrax, black pox, plague, toxic influenza, hemorrhagic exudative inflammation is diagnosed. The reasons for it are the increasing permeability of microvessels up to their ruptures. In this case, the exudate is dominated by erythrocytes, due to which its color varies from pink to dark red. The external manifestation of hemorrhagic inflammation is similar to hemorrhage, but, unlike the latter, not only erythrocytes are found in the exudate, but also a small proportion of neutrophils with macrophages. Treatment of hemorrhagic exudative inflammation is prescribed taking into account the type of microorganisms that led to it. The outcome of the disease can be extremely unfavorable if therapy is started late and ifthe patient's body does not have enough strength to resist the disease.
Catarrhal inflammation
A feature of this pathology is that the exudate with it can be serous, purulent, and hemorrhagic, but always with mucus. In such cases, a mucous secretion is formed. Unlike serous, it contains more mucin, the antibacterial agent lysozyme, and A-class immunoglobulins. It is formed for the following reasons:
- viral or bacterial infections;
- exposure to the body of chemicals, high temperatures;
- metabolic disorders;
- allergic reactions (eg allergic rhinitis).
Catarrhal exudative inflammation is diagnosed with bronchitis, catarrh, rhinitis, gastritis, catarrhal colitis, acute respiratory infections, pharyngitis and can occur in acute and chronic forms. In the first case, it is completely cured in 2-3 weeks. In the second, changes occur in the mucosa - atrophy, in which the membrane becomes thinner, or hypertrophy, in which, on the contrary, the mucosa becomes thickened and can protrude into the organ cavity.
The role of mucous exudate is twofold. On the one hand, it helps fight infection, and on the other hand, its accumulation in the cavities leads to additional pathological processes, for example, mucus in the sinuses contributes to the development of sinusitis.
Treatment of catarrhal exudative inflammation is carried out with antibacterial drugs, physiotherapeutic procedures and folk methods, such as heating, rinsing with various solutions,ingestion of infusions and decoctions of herbs.

Exudative inflammation: characterization of specific exudative fluids
Chylous and pseudochylous exudates were mentioned above, appearing with injuries of the lymphatic vessels. For example, in the chest, this may be with a rupture of the thoracic duct. Chylous exudate is white in color due to the presence of an increased amount of fat in it.
Pseudochylous also has a whitish tint, but it contains no more than 0.15% fat, but there are mucoid substances, protein bodies, nucleins, lecithins. It is observed in lipoid nephrosis.
White color and chyle-like exudate, only the decayed degenerate cells give it color. It is formed during chronic inflammation of the serous membranes. In the abdominal cavity, this happens with cirrhosis of the liver, in the pleural cavity - with tuberculosis, pleural cancer, syphilis.
If there are too many lymphocytes in the exudate (more than 90%), it is called lymphocytic. It is released from the vessels in pleural tuberculosis. If cholesterol is present in the secret, by analogy it is called cholesterol. It has a thick consistency, yellowish or brownish color and can be formed from any other exudative fluid, provided that water and mineral particles are reabsorbed from the cavity in which it accumulates for a long time.
As you can see, there are many types of exudates, each of which is characteristic of a certain type of exudative inflammation. There are also cases when, for any one disease,mixed exudative inflammation is diagnosed, for example, serous-fibrous or serous-purulent.

Acute and chronic forms
Exudative inflammation can occur in acute or chronic form. In the first case, it is an instant response to a stimulus and is designed to eliminate this stimulus. There can be many reasons for this form of inflammation. Most common:
- injury;
- infections;
- chemical poisoning;
- disturbances in the functioning of any organs and systems.
Acute exudative inflammation is characterized by redness and swelling of the injured area, pain, fever. Sometimes, especially due to infection, patients have symptoms of autonomic disorders and intoxication.
Acute inflammation is relatively short-lived, and if the therapy is carried out correctly, it is completely cured.
Chronic exudative inflammation can last for years. It is represented by purulent and catarrhal types of the inflammatory process. At the same time, tissue destruction develops simultaneously with healing. And although in the stage of remission chronic inflammation of the patient almost does not bother, it can ultimately lead to exhaustion (cachexia), sclerotic changes in the vessels, irreversible disruption of the organs and even to the formation of tumors. Treatment is mainly aimed at maintaining the remission phase. In this case, great importance is attached to the correct image.life, diet, immunity.