- Author Curtis Blomfield blomfield@medicinehelpful.com.
- Public 2023-12-16 20:44.
- Last modified 2025-01-23 17:01.
If a person has a large amount of fluid in the pleural cavity, this indicates the development of a pathological process in the body. To identify a violation, it is necessary to analyze the effusion in several directions. Below is information on what violations can be detected by the study, how to prepare for the collection of biomaterial and how to decipher the conclusion issued in the laboratory.
Indications
The pleural cavity is a small space that looks like a gap. It is located between the chest and lungs. The pleural cavity is a zone that plays an important role in the process of breathing. It produces a small amount of fluid, which is necessary to reduce the rate of friction of the lungs against the chest from the inside.
Normally, up to 25 ml of this lubricant is released. Against the background of the course of any pathological process, the production of fluid increases. Therebythe lung cannot fully expand when inhaled.
The main indication for the appointment of the analysis is an inexplicable increase in the amount of pleural fluid, combined with fever, shortness of breath, pain in the chest, cough and chills. Based on the results of the study, the doctor can judge the cause of the pathological condition.

What reveals
The accumulation of pleural fluid is a consequence of the course of many ailments. Main causes of effusion:
- Congestive heart failure.
- Cirrhosis of the liver.
- Atelectasis.
- Nephrotic syndrome.
- Mixedema.
- Adhesive form of pericarditis.
- Infiltration of cerebrospinal fluid into the pleura after injury or surgery.
- Displacement of the venous catheter (central).
- Duropleural fistula.
- Pneumonia.
- Tuberculosis.
- Malignant neoplasms.
- Occlusion of a pulmonary artery thrombus.
- Systemic lupus erythematosus.
- Rheumatoid pleurisy.
- Pancreatitis.
- Perforation of the esophagus.
- Infection of a fungal nature.
- Lung abscess burst.
- Meigs Syndrome.
- Ovarian hyperstimulation during IVF.
- Asbestosis.
- Severe renal failure of a chronic nature.
- Sarcoidosis.
- Pathologies of an autoimmune nature.
- Liver abscess.
Under analysisA pleural effusion specialist can detect the above diseases even at an early stage of their development.

Preparation
The decision regarding the advisability of a puncture is made by the attending physician based on the results of the diagnosis. If analysis of the pleural effusion is necessary, the specialist needs to prepare the patient for the upcoming procedure.
First of all, the doctor refers the patient for an examination, including:
- ECG.
- X-ray.
- Ultrasound.
If the patient has a severe cough, the doctor prescribes him medication.
Immediately before the procedure, the nurse measures the patient's pulse and pressure. In addition, a clinical blood test is performed. If the patient is unconscious, the procedure is carried out in the stadium ward. In other cases, it is carried out in the manipulation room.

Biomaterial sampling algorithm
Pleural fluid puncture is a serious procedure that requires certain skills from the doctor.
Algorithm for its implementation:
- The patient takes a sitting position and rests his hands on the back of the chair. Less often, the patient is laid on the couch and turns on a he althy side. At the same time, he should put his hand behind his head.
- A nurse measures blood pressure and pulse. She must monitor the indicators throughout the entire procedure. If abnormalities are detected, she must notify the doctor about this.
- Specialist examines x-ray to determine the puncture site. With the accumulation of pathological effusion, the needle is inserted in the zone 7-9 of the intercostal space along the axillary line from behind. If the patient is in the supine position, the puncture site is slightly displaced.
- The skin around the required area is covered with disposable sterile diapers. Then the puncture site is treated with alcohol or iodine solution.
- Doctor administers anesthesia. As a rule, novocaine solution is used for the purpose of anesthesia. The needle is inserted along the upper part of the underlying rib. This reduces the risk of damage to blood vessels and nerve fibers to a minimum. The solution is injected gradually.
- The doctor pierces the pleura with a disposable sterile needle. The patient at this time experiences sharp painful sensations. The pleural fluid enters the syringe by pulling the plunger. With a large amount of effusion, an electric pump is used. In such cases, the needle is replaced with a thicker one.
- After pumping out the effusion, the doctor injects an antimicrobial drug into the pleural cavity.
The final step is to sharply remove the needle. The puncture site is then treated with iodine solution or medical alcohol. After that, a bandage or plaster is applied to it.

Possible Complications
It is important to know that the puncture is associated with certain risks. With the correct procedure, it is minimal.
In rare cases, complications develop that require immediate medical attention (includingsurgical). These include:
- Injury to lung tissue resulting in pneumothorax.
- Puncture of the stomach, diaphragm, liver or spleen. These conditions instantly disrupt the heart and can lead to cardiac arrest.
- Violation of the integrity of blood vessels.
- Infection of the pleura or chest.
- Air embolism of cerebral blood vessels.
- Dramatic decrease in blood pressure.
If a patient coughs up blood, becomes very pale, loses consciousness, or has convulsions, the person is taken to the intensive care unit.
Macroscopic study
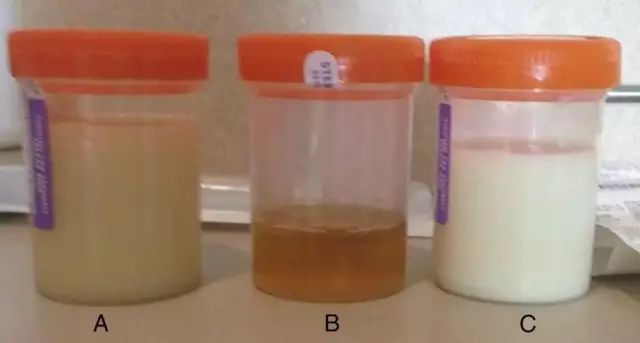
This analysis of the pleural fluid involves its assessment of the nature, density, transparency and color.
Doctors divide effusion into 2 large groups:
- Transudates. These are non-inflammatory fluids.
- Exudates. These are inflammatory effusions. They, in turn, can be serous, serous-fibrinous, hemorrhagic, chylous, chyle-like, pseudo-chylous, cholesterol, putrefactive.
Indicators of the color and transparency of the pleural fluid in the lungs directly depend on its nature. Serous exudates and transudates are usually light yellow in color. At the same time, they are transparent. Other types of exudates are cloudy and may have different colors.
The density of the liquid is determined by the urometer. In transudates, the indicator ranges from 1005-1015, in exudates - above 1015.

Chemical Research
In the process of analysis, the protein content is determined using a refractometer. The indicator is measured in grams per liter. Transudates contain up to 25 g/l, exudates - more than 30 g/l.
In order to differentiate liquids, a Riv alta test is performed. The essence of the method is to acidify distilled water, followed by adding a few drops of effusion to it. Exudates in the process of a chemical reaction form turbidity, resembling an outwardly white cloud. Its appearance is due to the presence of seromucin in the liquid - a substance that coagulates upon contact with acetic acid. Transudates do not have this property, that is, they do not form opacities.
Microscopic analysis
This is a pleural fluid test that evaluates the cellular composition of the effusion:
- Fat drops. Characteristic of purulent and chylous exudates.
- Crystals of cholesterol. Present in old effusions.
- Malignant cells.
- Erythrocytes and leukocytes. Normally, they are present in all fluids. An increased number of erythrocytes and leukocytes may indicate the presence of purulent and serous exudate.
- Mesothelial cells. If they have undergone changes and are found in the form of clusters, this indicates an old transudate.

Duration
Analysis of pleural fluid takes time. In most cases, the patient receives a conclusion 3 working days after the collectionbiomaterial. The procedure itself takes no more than 30 minutes.
Interpretation of results
A normal pleural effusion is clear and colorless. The pH of the liquid is not less than 7.6 and not more than 7.64. The protein content in the exudate should not exceed 2 g/l. The number of leukocytes is normally not more than 1000 mm3. The glucose level is the same as in the blood. The level of LDH is 2 times less than in liquid connective tissue.
Any deviation from the norm indicates violations:
- Red effusion - pulmonary infarction, asbestosis, trauma, malignancy, pleural endometriosis.
- Milky or white shade - tumor metastasis, lymphoma.
- Black color - the body is infected with the fungus aspergilus.
- Greenish tint - the presence of a fistula between the gallbladder and the pleural cavity.
- Dark red or brown - amoebiasis, ruptured liver cyst.
- Viscous effusion - empyema, mesothelioma.
- A pH value of less than 6 indicates damage to the esophagus.
- PH level 7-7, 2 - pleurisy.
- pH value 7, 3 - empyema, tumor, systemic lupus erythematosus, tuberculosis, violation of the integrity of the walls of the esophagus. In addition, such an indicator often indicates pleurisy of a rheumatoid nature.
- High level of LDH (1000 units or more) - a malignant tumor, empyema, pneumonia (usually against the background of AIDS), paragonimiasis.
- Glucose less than 1.6 mmol/l - rheumatoid pleurisy. Less often - empyema.
- Glucose level from 1, 6up to 2, 7 mmol / l - tumor, rupture of the esophagus, pleurisy against the background of systemic lupus erythematosus, tuberculosis.
- The presence of lactic acid indicates the active life of bacteria.
- Presence of amylase in effusion - pancreatitis, violation of the integrity of the walls of the esophagus, pancreatic pseudocyst, necrosis of the small intestine, peptic ulcer.
- Elevated level of neutrophils - empyema, infectious diseases.
- Increase in red blood cells - tumors, chest injuries, pulmonary infarction.
- Lymphocytes over 85% - tuberculosis, sarcoidosis, lymphoma, chronic rheumatoid pleurisy, chylothorax, yellow nail syndrome.
- Presence of abnormal cells - tumor metastasis, mesothelioma, blood cancer.
- Lymphocytes not less than 50 and not more than 70% - the presence of a malignant neoplasm.
- Eosinophils more than 10% - asbestosis, pulmonary embolism, parasitic or fungal diseases, tumor.
Thus, by analyzing the pleural fluid, it is possible to identify the existing pathology at any stage of its development.

Where to return
Effusion testing is done in both public and commercial he alth facilities. But the analysis is not carried out in all clinics. The institution must have an equipped laboratory, reagents, as well as highly qualified workers. Regarding the availability of this service, you need to find out directly at the registry.
Cost
Price of pleural analysisFluids vary by region and facility policy. For example, the average cost of research in Moscow is 750 rubles. 23 laboratories in the capital are equipped with the necessary equipment and reagents. The lowest price in Moscow is 550 rubles, the highest is 950 rubles.
In addition, it is important to consider the cost of biomaterial sampling. The price is, on average, 250 rubles. In private institutions, a consultation with a doctor is additionally paid. The cost of the initial appointment varies from 1000 to 2500 rubles.
At the polyclinic of the place of residence, the analysis of pleural fluid (if this service is available) is carried out free of charge, you only need to present a medical insurance policy.
In closing
Examination of effusion is indicated with a sharp increase in its volume. By analyzing the pleural fluid, the doctor is able to detect the presence of a pathological process even at an early stage of its development. The study does not imply compliance with strict preparation rules, all the necessary activities are carried out by the doctor and nurse immediately before the procedure.
Effusion puncture is associated with pain in the patient. In order to minimize them, the doctor injects a person with a solution of novocaine. After that, biomaterial is taken. The duration of the procedure is about half an hour.